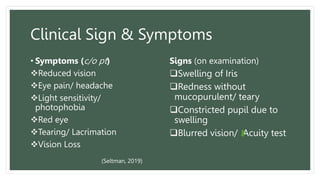
The document provides an overview of medical and surgical nursing concerning iritis and corneal ulcers, detailing the anatomy and physiology of the eye, as well as the pathophysiology, symptoms, diagnosis, and management of these conditions. It emphasizes the importance of early diagnosis and treatment to prevent complications such as vision loss and highlights the nursing care process for managing patient pain and anxiety. Health education and lifestyle modifications are also discussed in relation to preventing these ocular conditions.