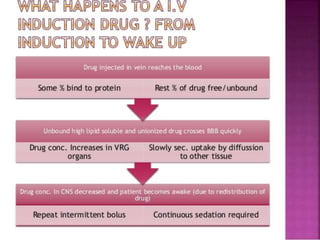
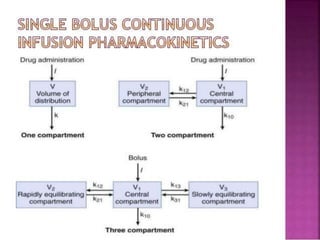
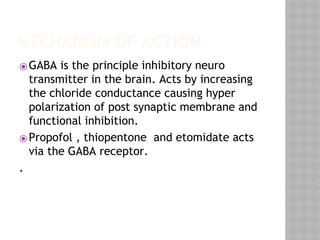
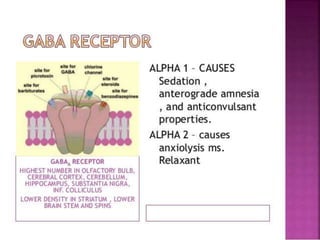
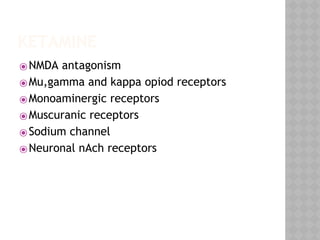
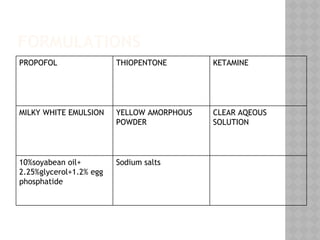
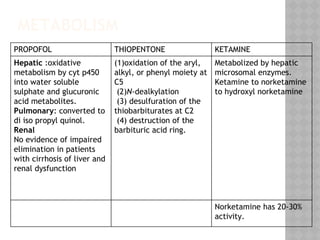
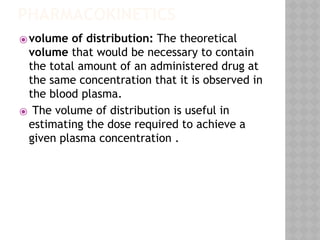
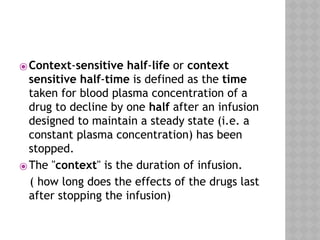
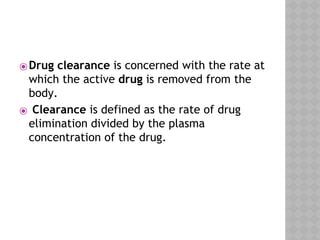
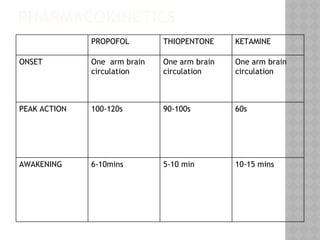
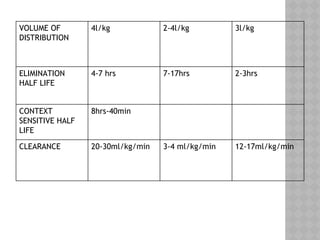
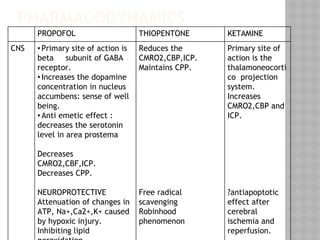
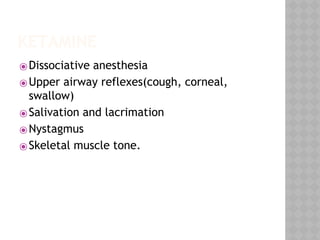
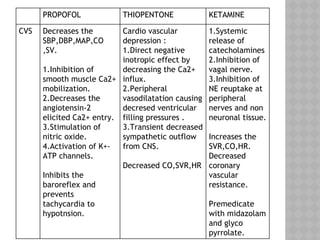
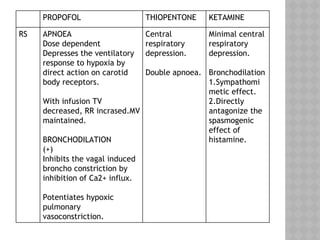
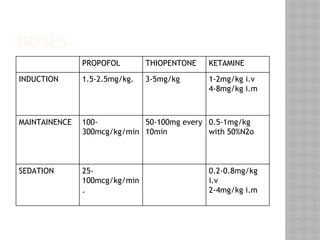
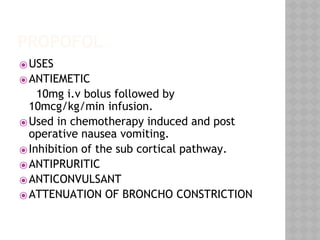
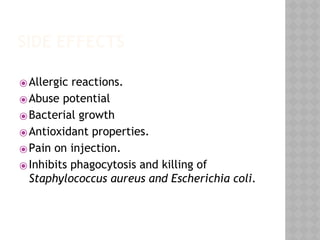
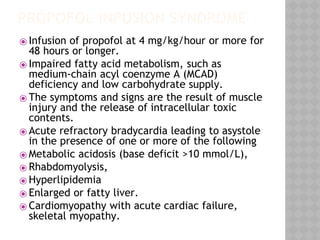
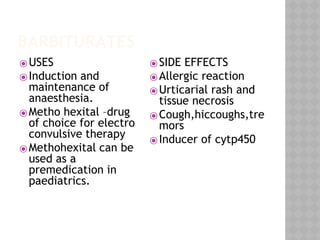
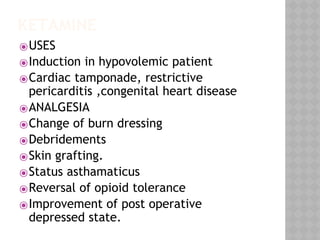
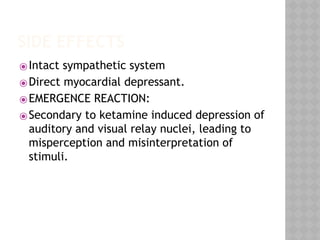
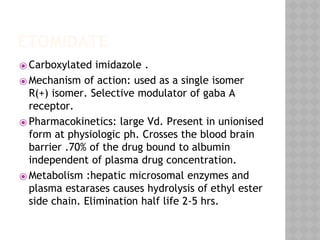
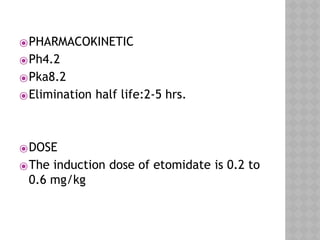
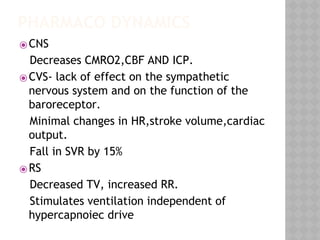
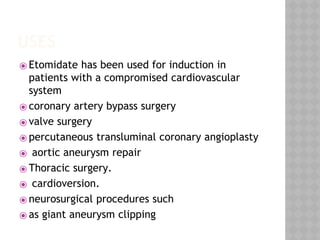
This document summarizes the pharmacokinetics and pharmacodynamics of common intravenous anesthetic agents. It discusses the mechanisms of action, metabolism, and effects of propofol, thiopental, ketamine, etomidate, and barbiturates on the central nervous system, cardiovascular system, and respiratory system. It also provides information on their uses, dosages, and side effects. The document is presented by Dr. Suchetha S with Dr. Sagar S.M as moderator and Dr. Arun Kumar A as head of department.