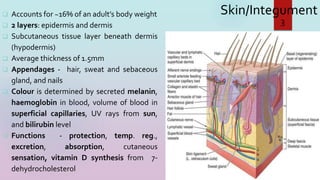
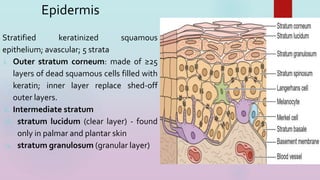
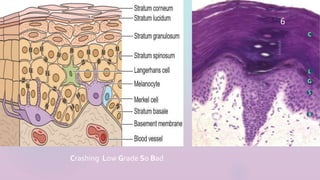
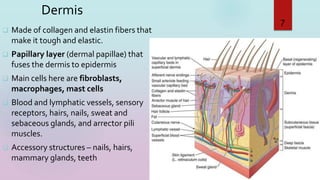
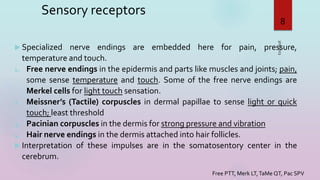
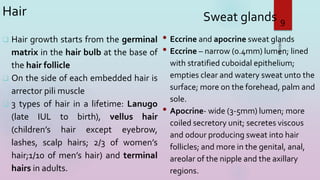
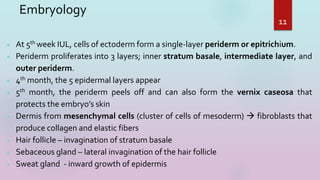
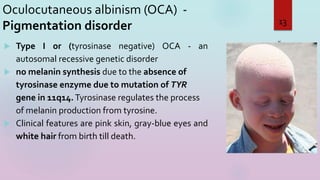
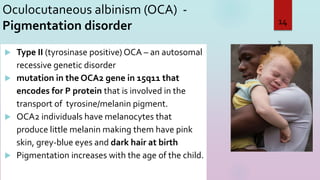
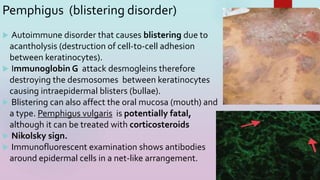
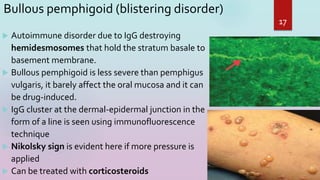
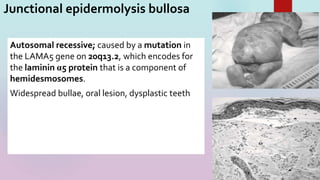
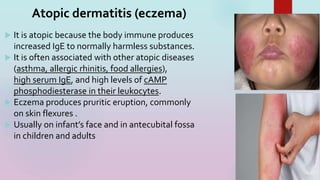
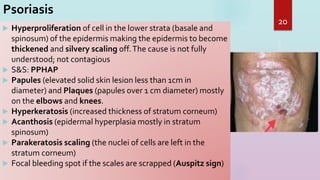
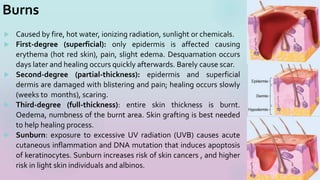
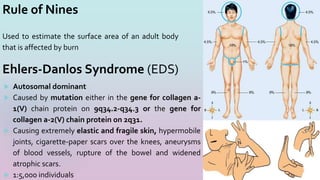
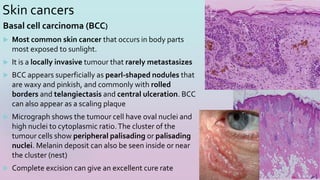
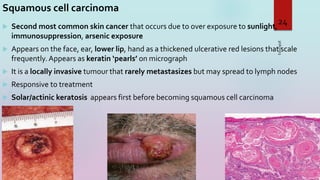
The document discusses the integumentary system, including the layers of the skin, skin appendages, embryology, sensory receptors, and various clinical correlates involving the skin. Specifically, it covers the epidermis, dermis, subcutaneous tissue, hair follicles, sweat glands, embryological development of the skin, sensory receptors, and highlights several conditions like burns, skin cancers, eczema, and psoriasis. The learning objectives are to understand the histology of the skin layers, embryology of the skin and glands, and clinical correlates related to skin pathology.