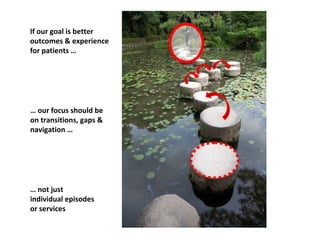
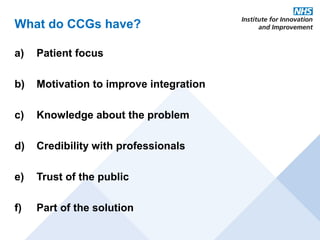
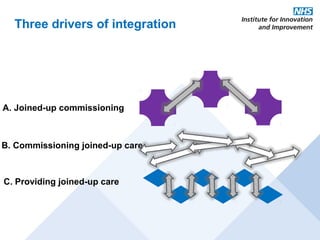
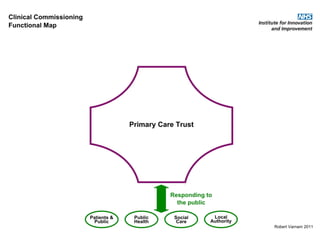
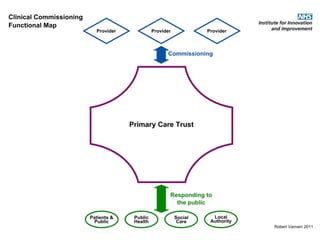
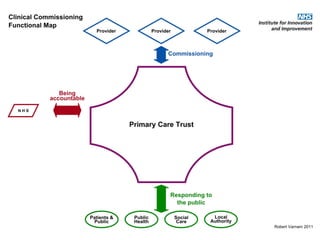
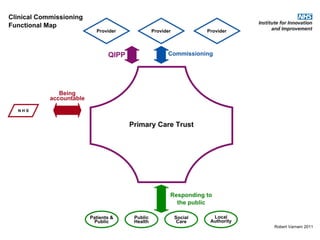
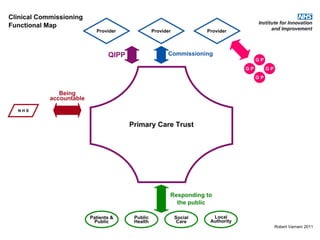
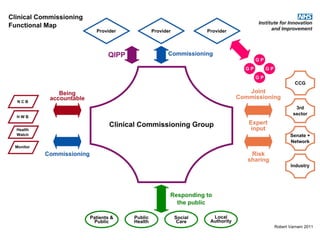
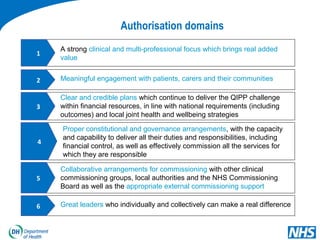
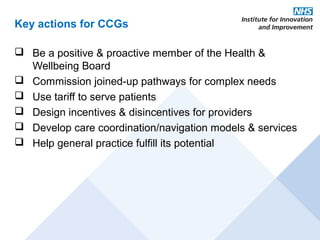
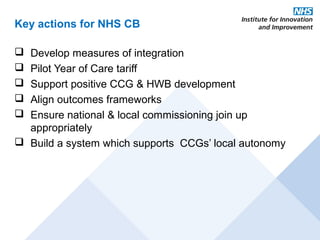
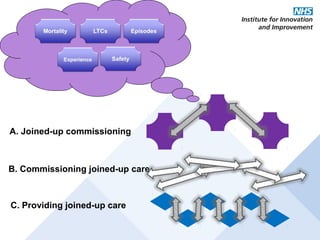
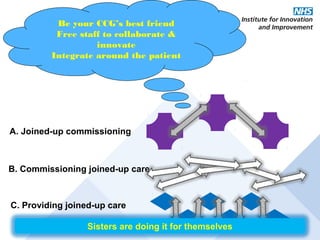
This document discusses commissioning and integration from the perspective of a clinical lead for primary care and commissioning. It outlines three key drivers of integration: (1) joined-up commissioning, (2) commissioning joined-up care, and (3) providing joined-up care. It emphasizes that clinical commissioning groups are well-positioned to improve integration and outcomes for patients by focusing on transitions between services, addressing gaps, and improving navigation for patients.