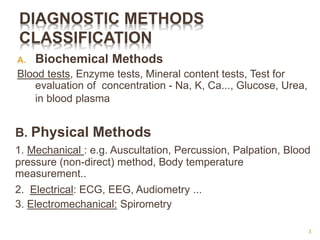
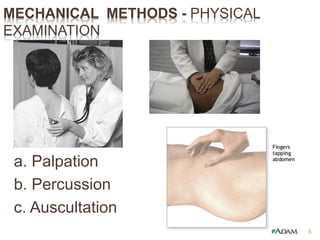
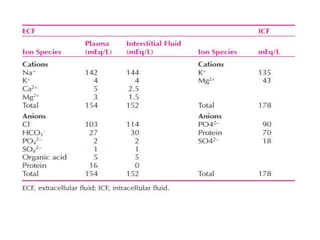
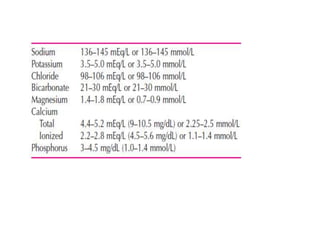
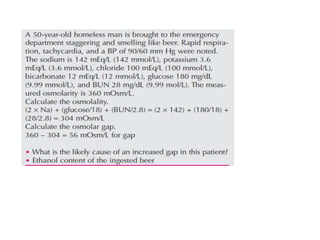
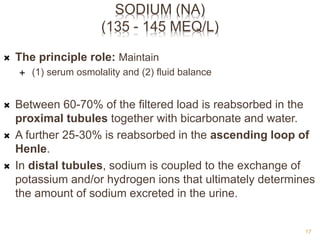
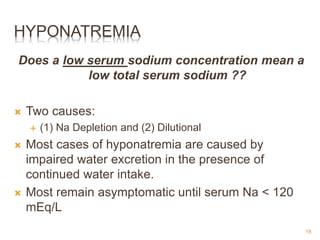
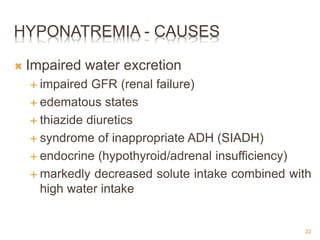
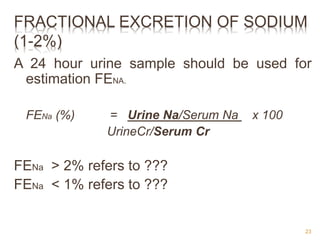
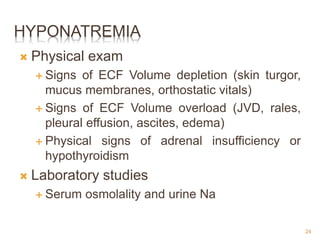
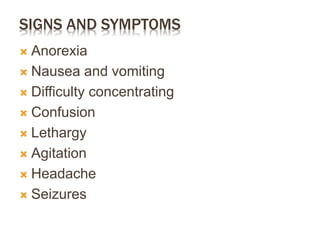
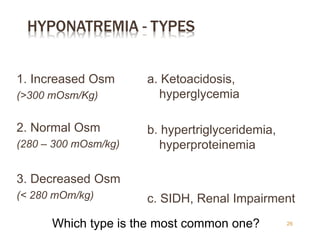
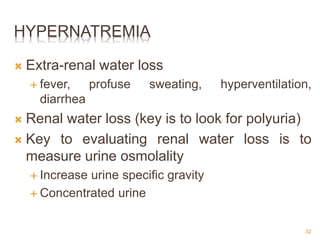
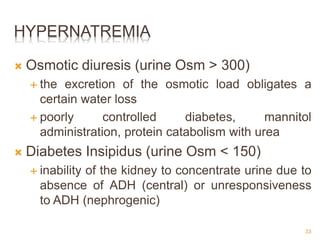
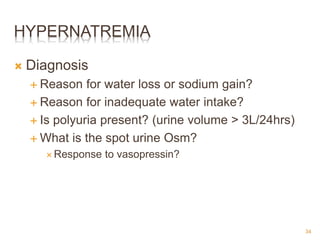
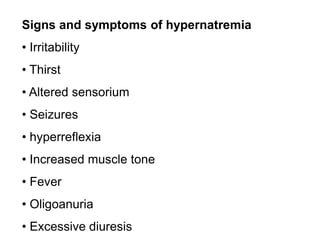
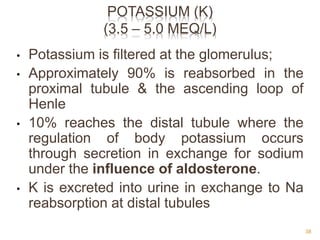
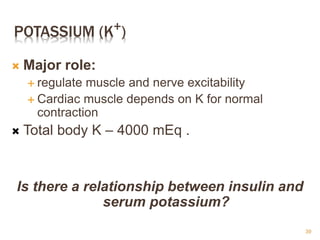
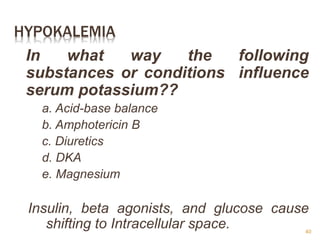
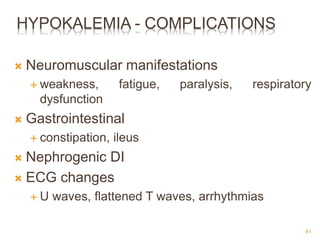
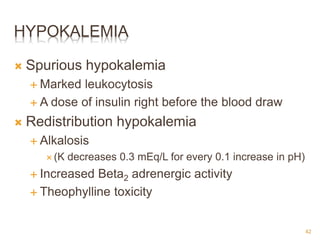
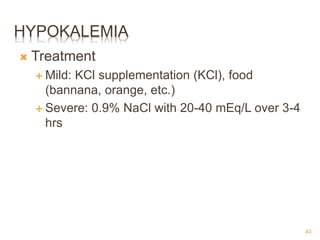
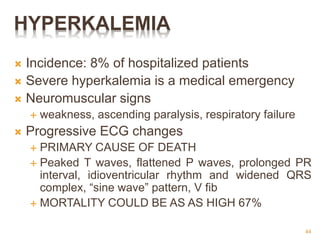
This document provides an overview of common laboratory tests interpreted by pharmacists, including their purpose, normal values, and clinical significance. It discusses electrolyte tests such as sodium, potassium, and their imbalances. Sodium is important for fluid balance and osmolality. Hyponatremia can be dilutional or depletional, while hypernatremia results from water deficit. Potassium regulates muscle function and its levels are influenced by acid-base balance and medications like diuretics. The document also reviews other diagnostic methods like physical exams, ECG, and biochemical tests of blood and urine.
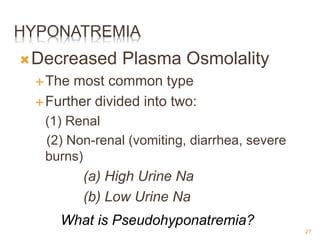
![HYPONATREMIA
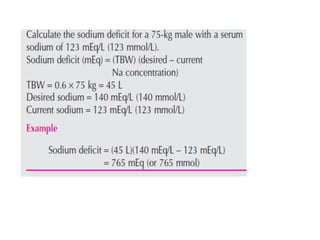
ACUTE, SYMPTOMATIC HYPONATREMIA
Calculate the Na deficit
Na mEq = ([Na desired] - [Na measured]) X TBW
TBW = 0.5 or 0.6 X weight in KG
Correct no faster than 1 mEq/L per hour for the first 6-8
mEq/L – No more than 10-12 mEq/L in first 24 hours
5% saline is almost never needed
How about in patients with
hypervolemic hyponatremia ???
28](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-28-320.jpg)
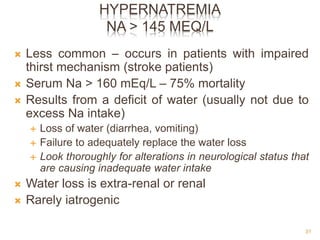
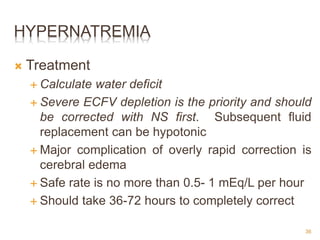
![HYPERNATREMIA
Treatment
Calculate the water deficit
H2O deficit = TBW X ([Na measured]- [Na desired])
[Na desired]
Important to take into account ongoing losses
insensible losses 0.5 - 1 liter/24 hours
with fever, these losses increase by 60-80ml/24 hrs for
each degree Fahrenheit
37](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-37-320.jpg)
![REGULATION OF PTH
Which one stimulates PTH secretion?
a. Low serum [Ca+2]
b. High serum [Ca+2]
54](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-54-320.jpg)
![HYPOALBUMINEMIA
To estimate the physiologic levels of
ionized calcium in states of
hypoalbuminemia:
[Ca+2]Corrected = [Ca+2]Measured + [ 0.8 (4 – Albumin) ]
Serum Ca (8 mEq/L) and Albumin is 2.5 g/dL.
What is the corrected Ca concentration?
57](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-57-320.jpg)

![CREATININE CLEARANCE
Creatine Clearance (CrCl)
[140 – age (yr)] x Wt (kg) x 0.85 (for women)
72 x SCr (mg/dl)
84](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-84-320.jpg)
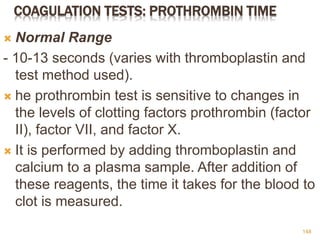
![CONT’D…
INR = [(Patient PT)/(Mean Normal PT)]ISI
INR 2.0-3.0
Atrial fibrillation
DVT treatment
PE treatment
Prophylaxis of venous thrombosis
Tissue heart valves
Valvular heart disease
Mechanical heart valves (certain types only) 150](https://image.slidesharecdn.com/interpretationlab-220530030429-67aaafa6/85/Integrated-Therapeutics-I-pptx-150-320.jpg)