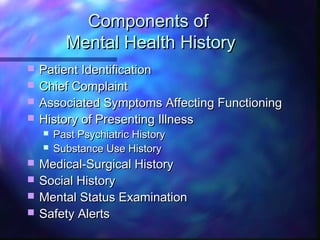
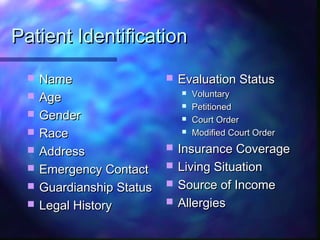
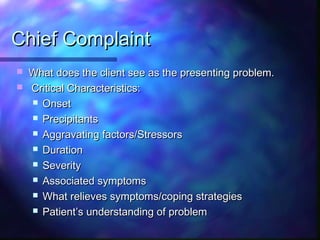
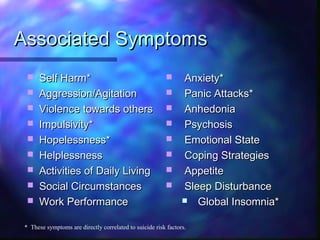
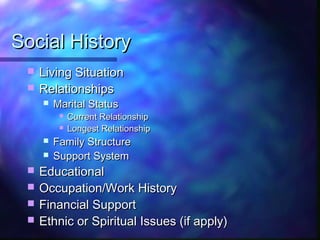
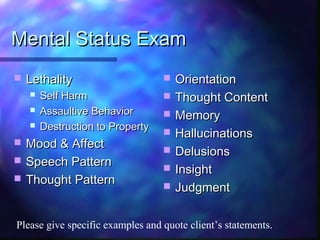
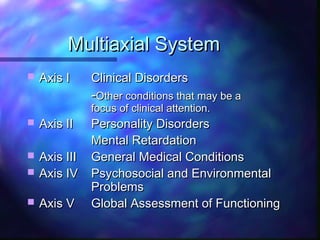
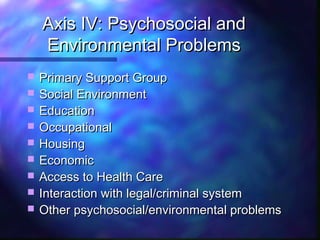
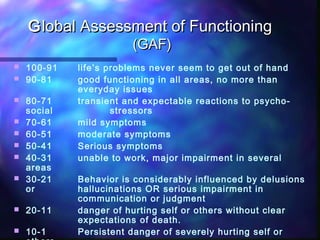
The document outlines the components of an initial psychiatric assessment, including patient identification, chief complaint, history of presenting illness, past psychiatric and medical history, social history, mental status examination, and safety alerts. It describes collecting information on symptoms, functioning, treatment, and stressors across multiple domains to inform a diagnosis and care plan. The assessment aims to evaluate severity of illness and care needs using a standardized multiaxial system and global assessment of functioning scale.