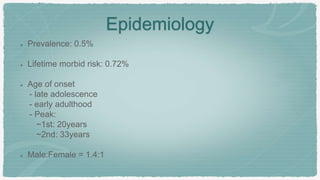
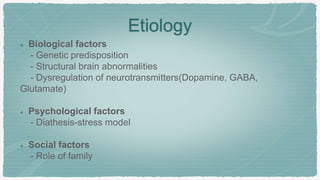
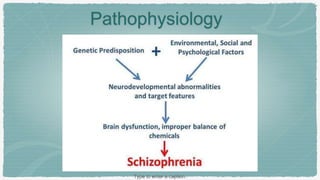
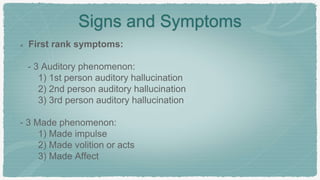
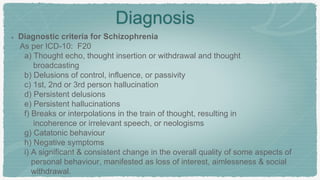
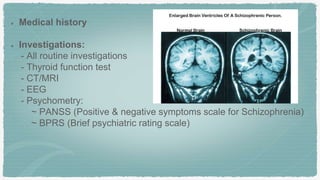
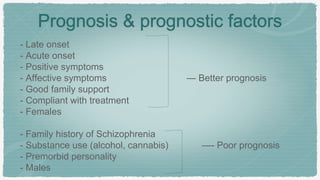
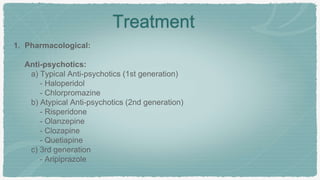
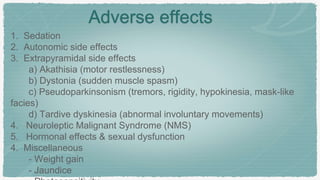
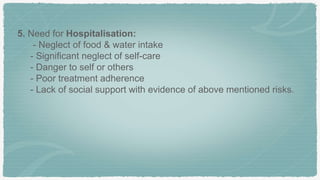
Schizophrenia is a mental disorder characterized by splitting of psychic functions and disturbed harmony between thought, emotions, and behavior. It has a prevalence of 0.5% and typically onset is in late adolescence or early adulthood. Etiology involves genetic, biological, and environmental factors. Symptoms include positive symptoms like delusions and hallucinations, negative symptoms such as social withdrawal, and cognitive impairment. Diagnosis involves meeting criteria for symptoms lasting at least 6 months from scales like PANSS. Treatment involves atypical antipsychotic medication which can have side effects as well as psychosocial therapies and hospitalization if risks are present.