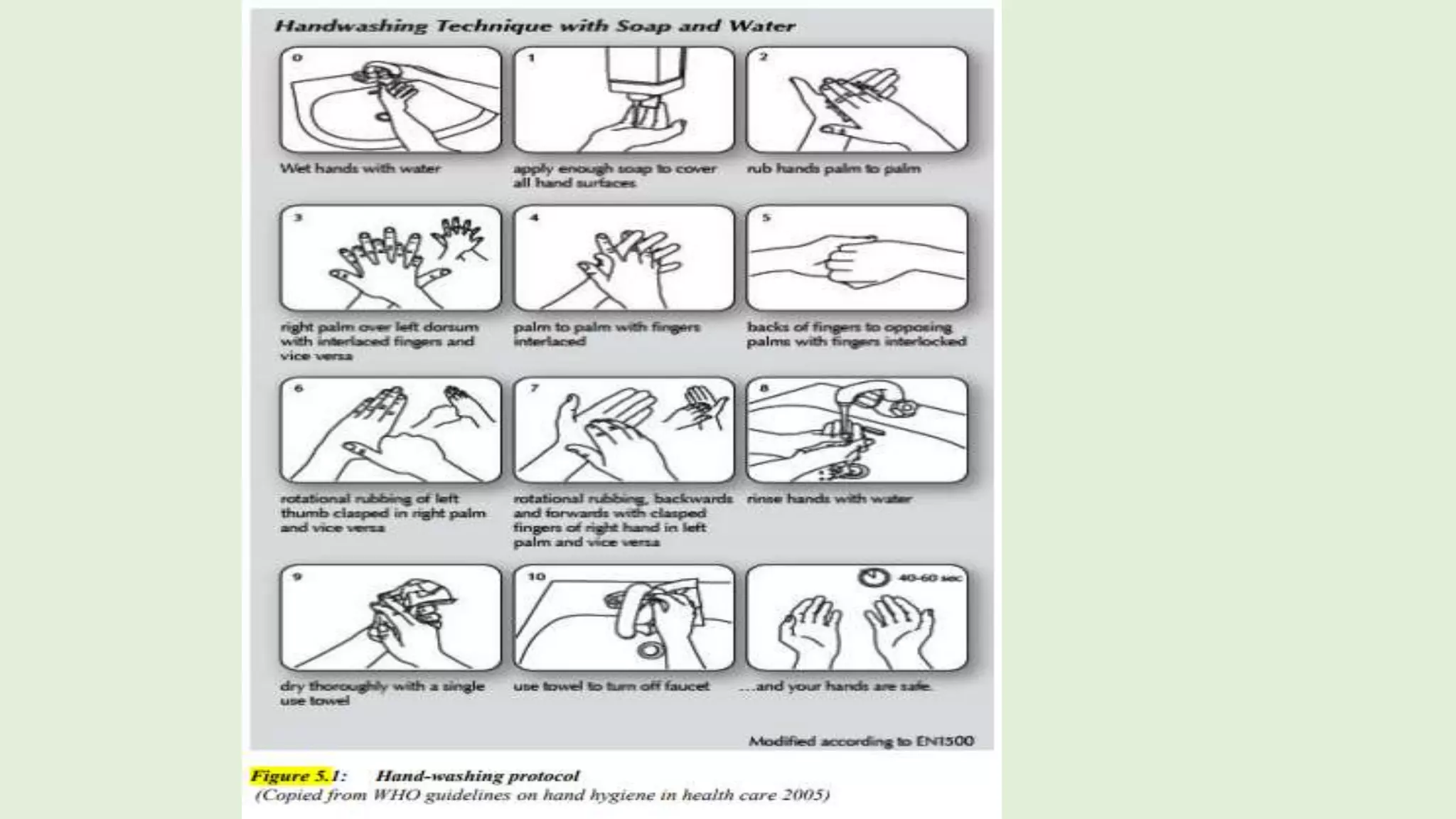
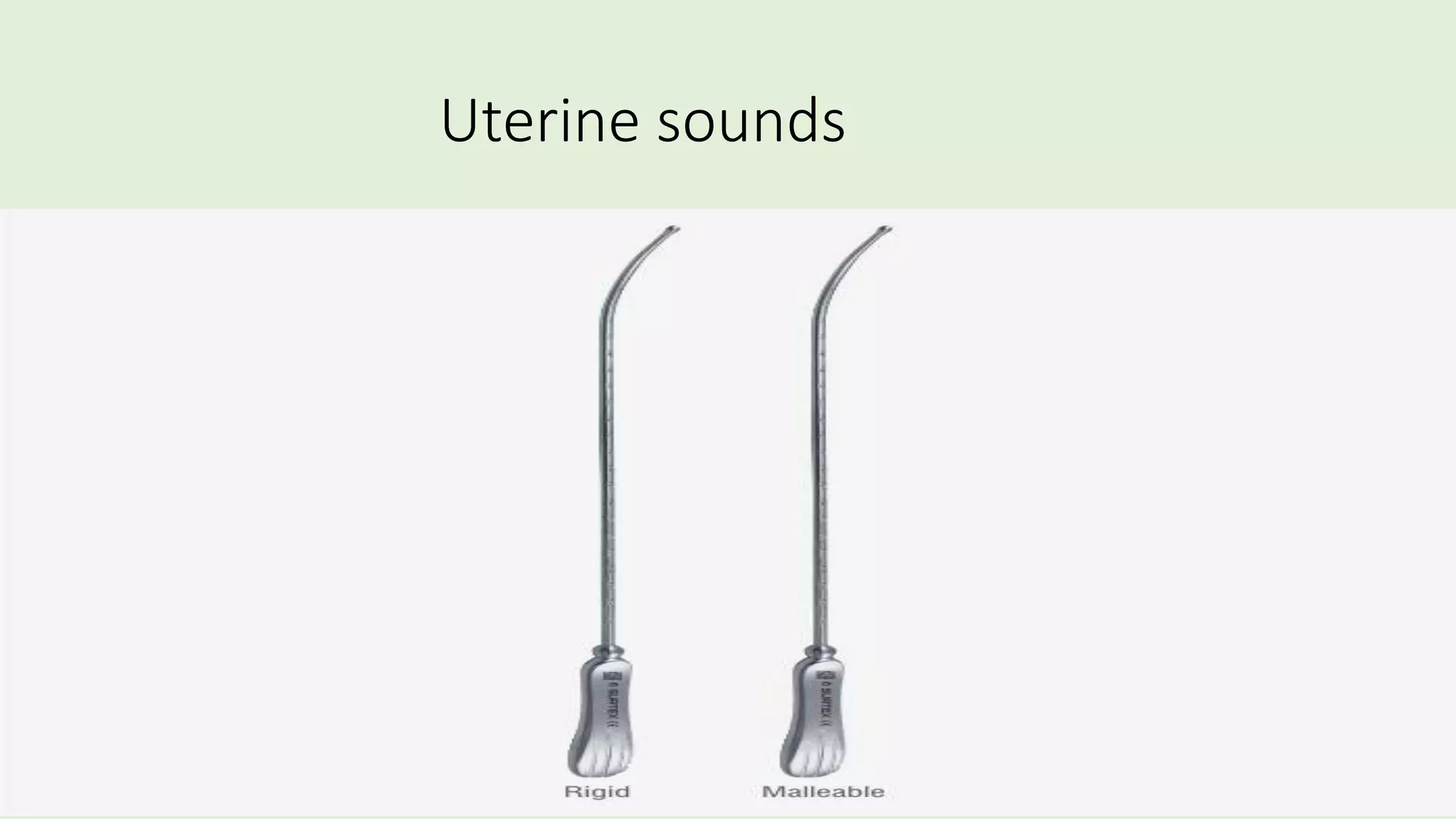
This document outlines basic infection prevention procedures for family planning clinics. It discusses common infectious organisms like bacteria, viruses, fungi and parasites. Basic rules include washing hands, properly processing reusable instruments, wearing gloves, only doing pelvic exams when necessary, using new auto-disable syringes and needles for injections, cleaning surfaces with chlorine solution, safely disposing of waste, and washing linens. Adhering to universal precautions is important to prevent the spread of infections between clients and communities.