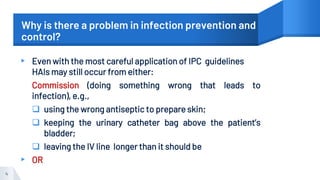
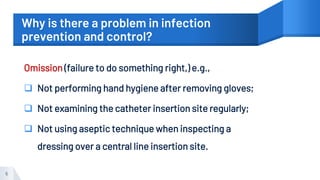
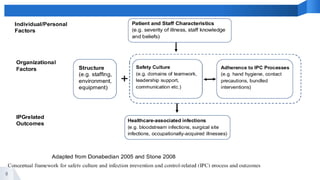
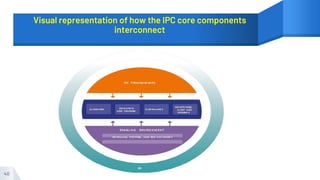
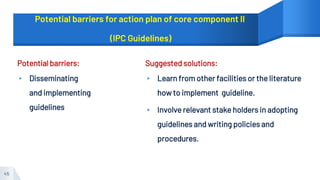
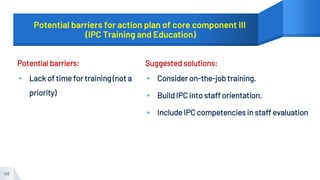
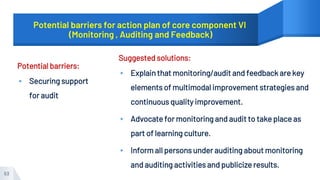
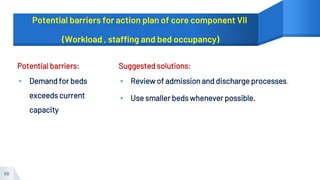
This document outlines the core components of an infection prevention and control (IPC) program according to the World Health Organization (WHO). It discusses eight core components: 1) IPC program structure, 2) evidence-based guidelines, 3) education and training, 4) surveillance of healthcare-associated infections, 5) multimodal strategies, 6) monitoring and audit, 7) adequate staffing and bed occupancy, and 8) appropriate facilities and equipment. For each component, it describes what should be included, who is responsible, and how it should be implemented. It also identifies potential barriers to implementing the components and provides suggested solutions.