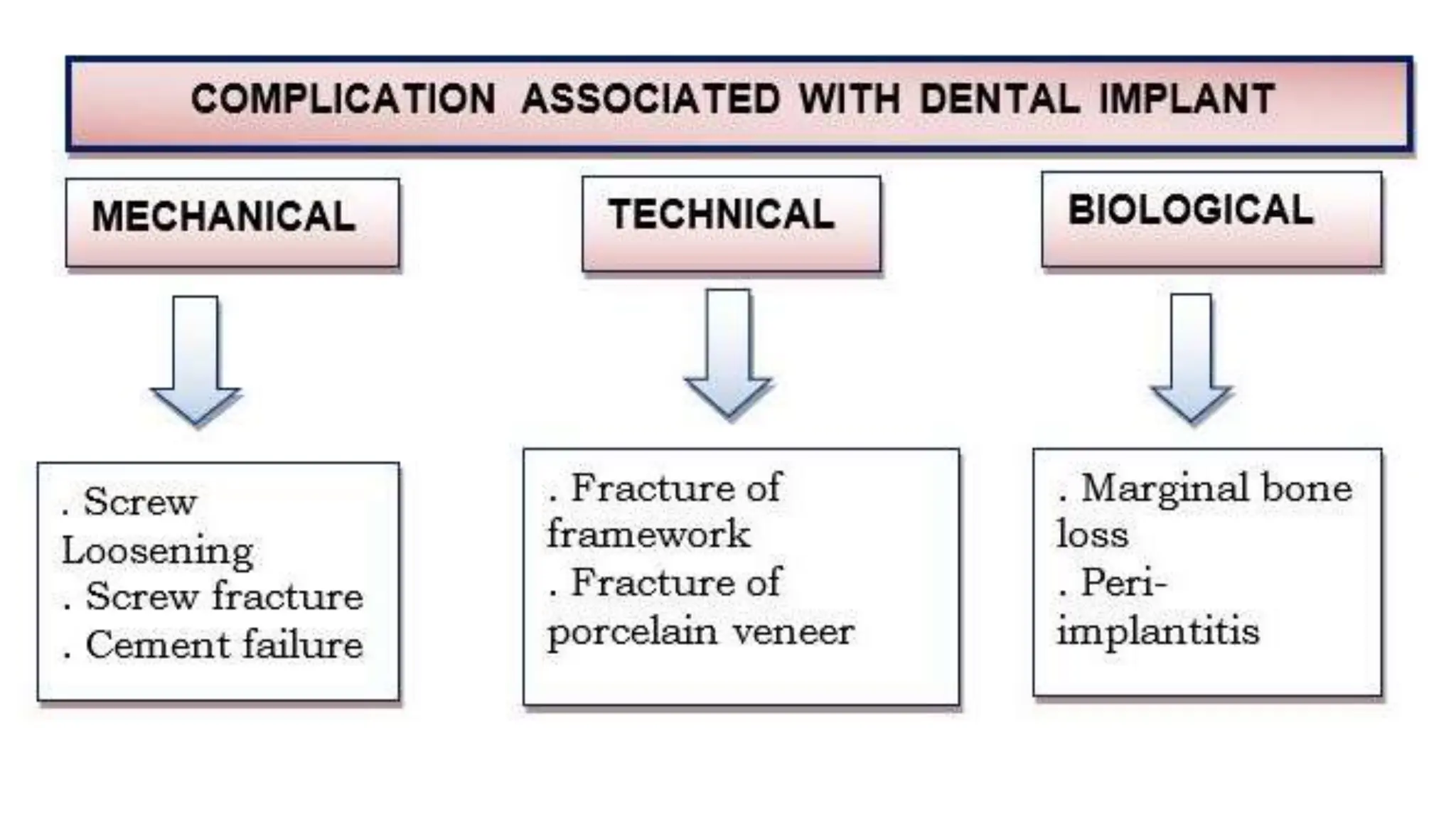
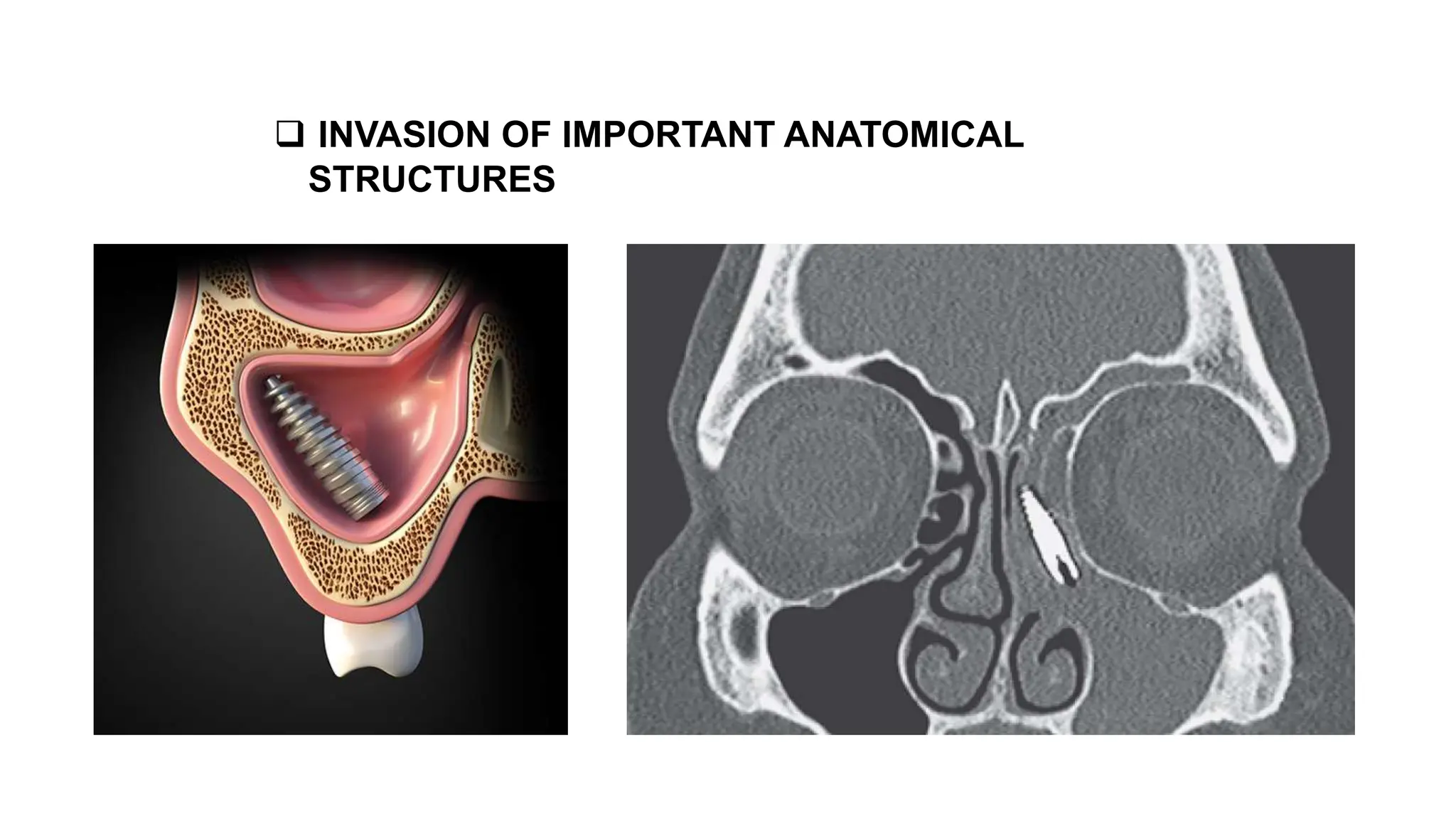
This document provides guidance on proper suturing techniques and preventing complications during dental implant surgery. It discusses:
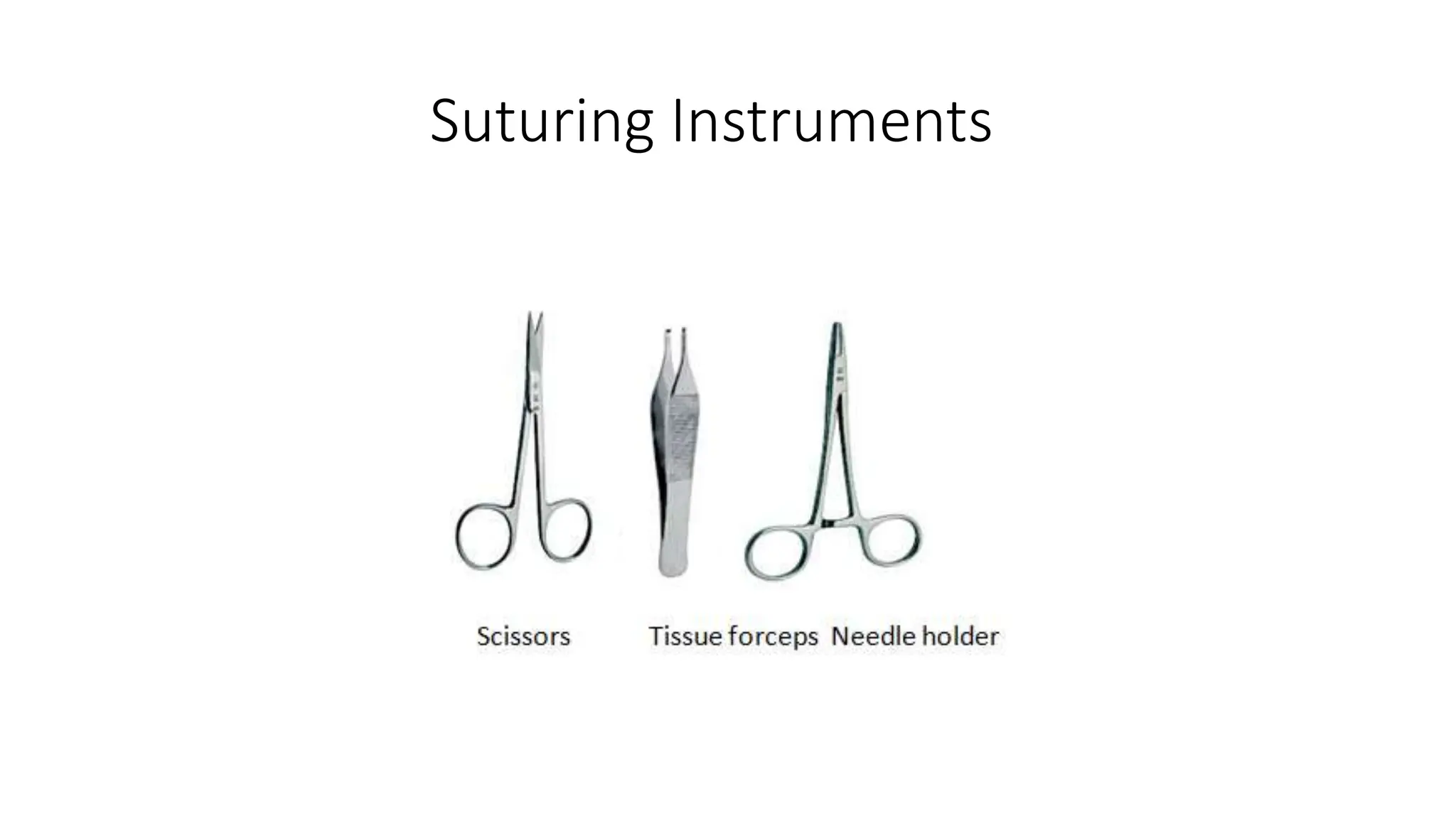
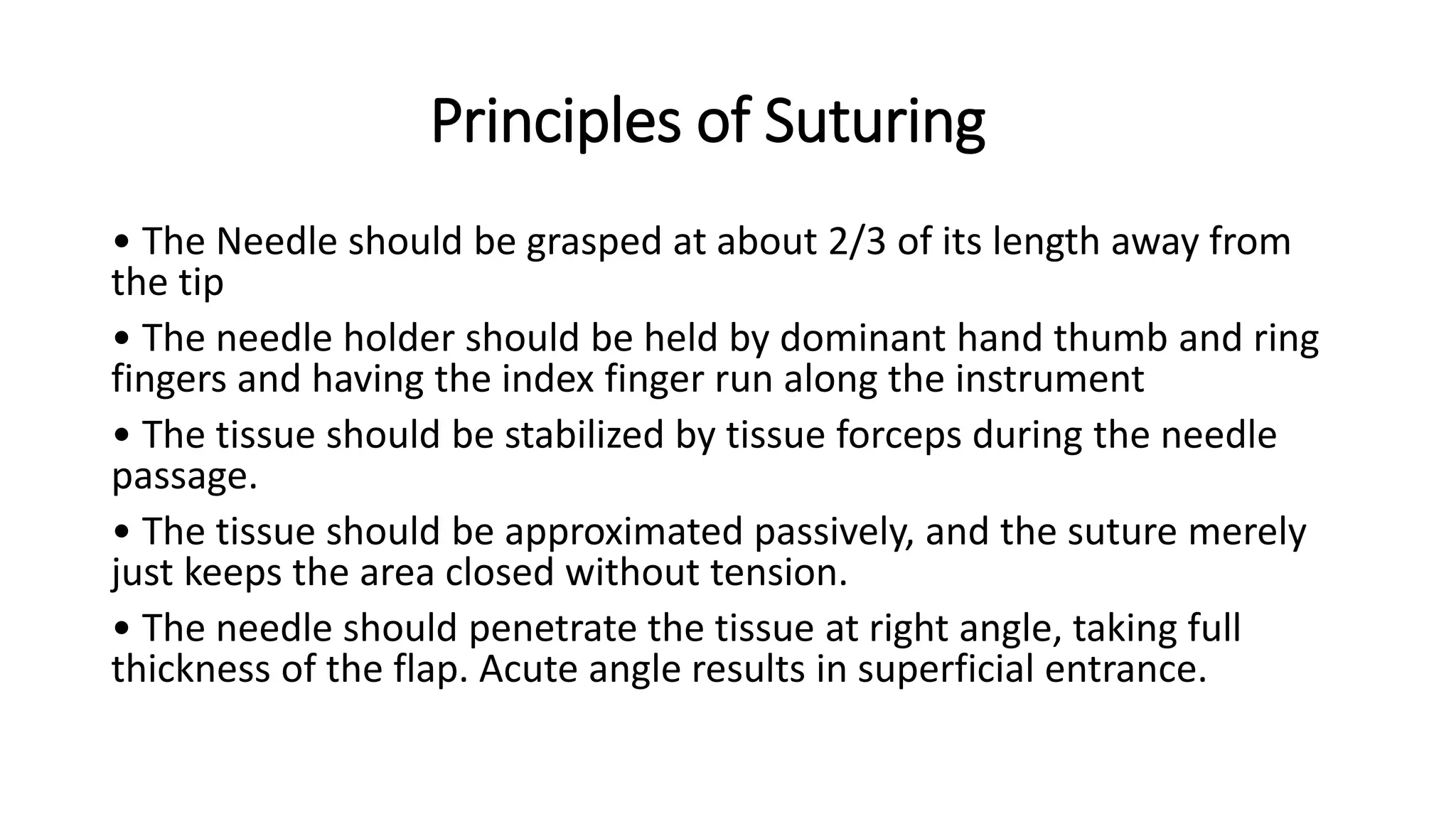
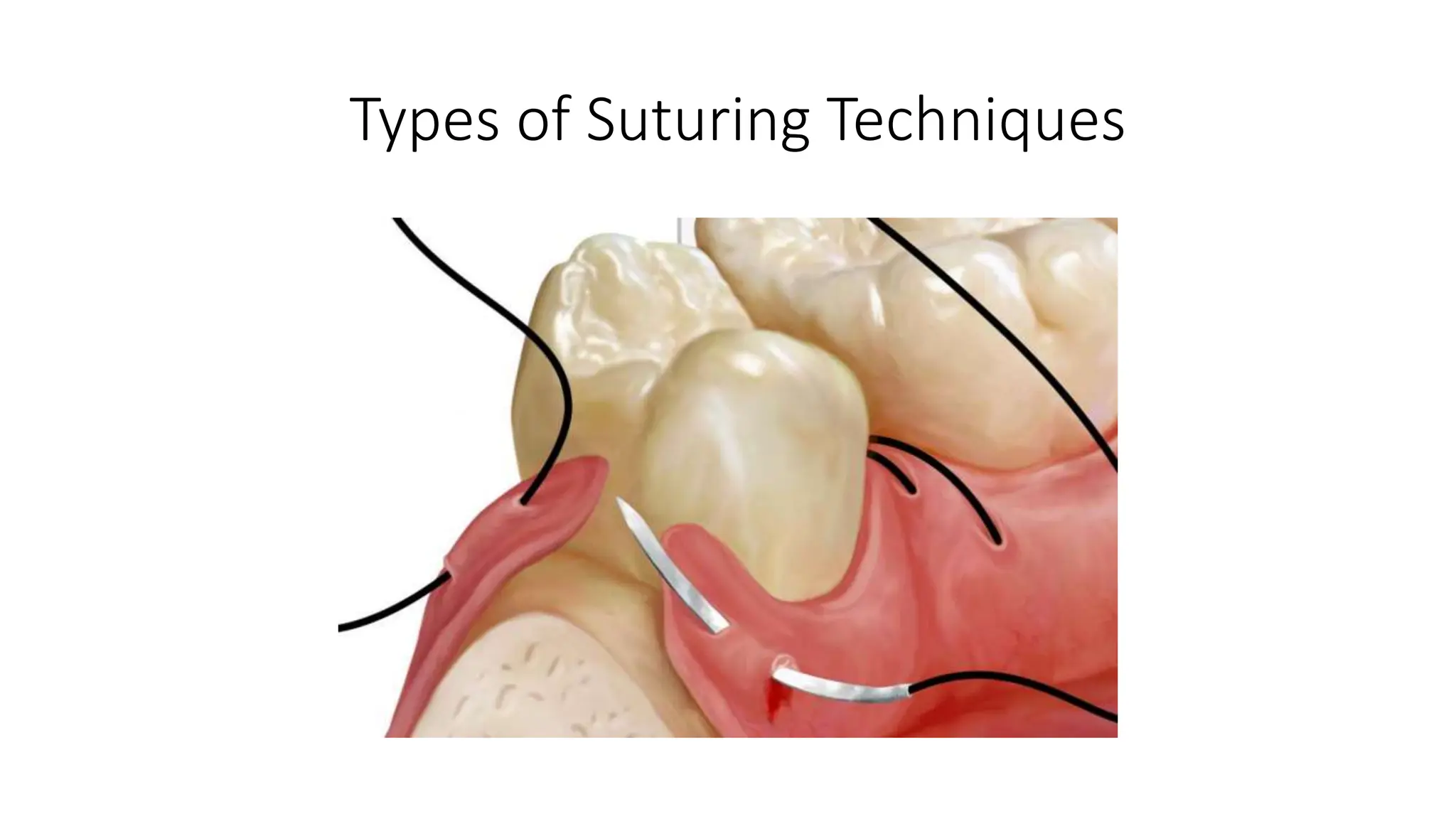
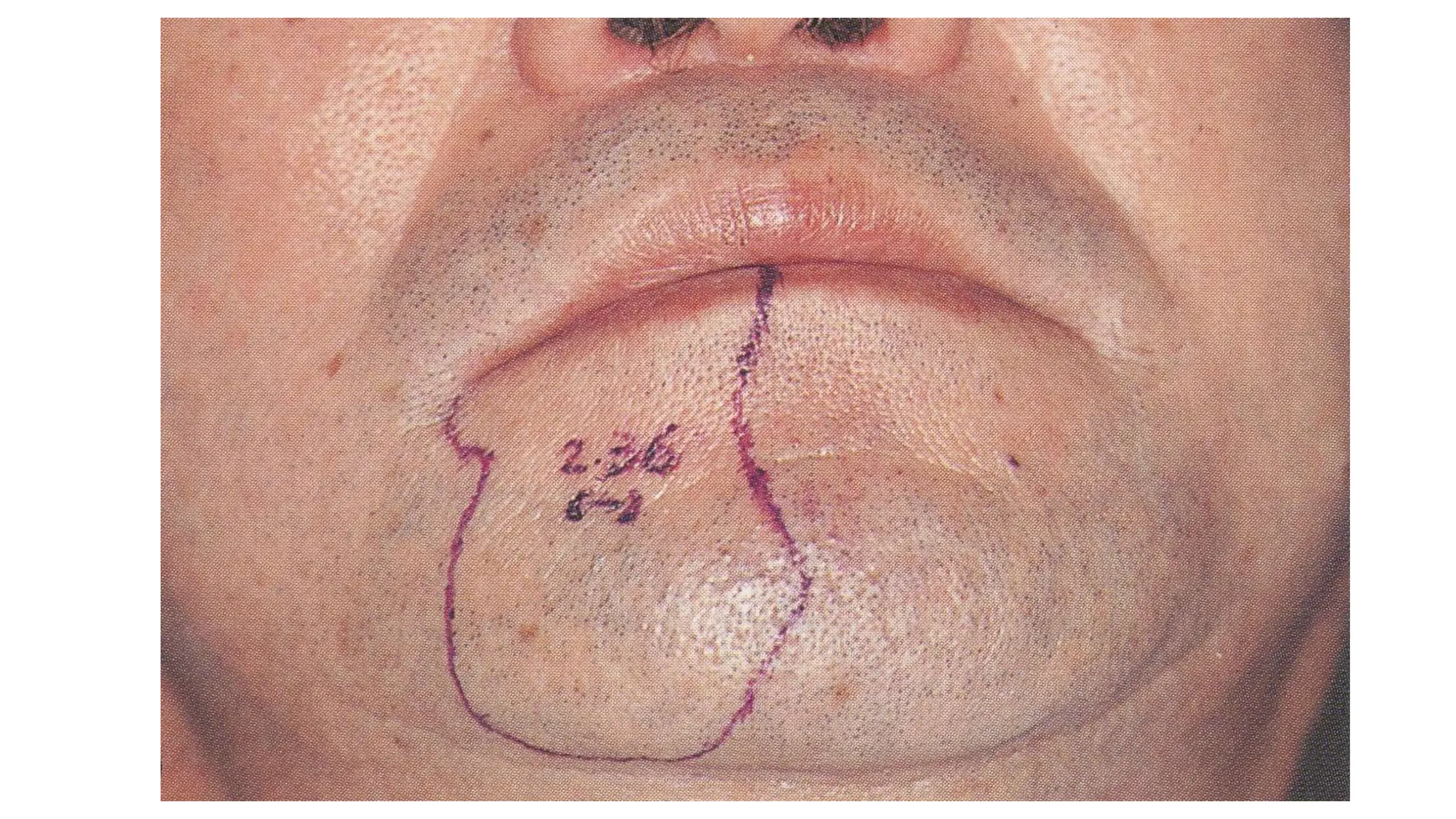
- Correct suturing techniques like grasping the needle at 2/3 its length away from the tip, stabilizing tissue with forceps, and passing the needle at a 90 degree angle through the full thickness of tissue.
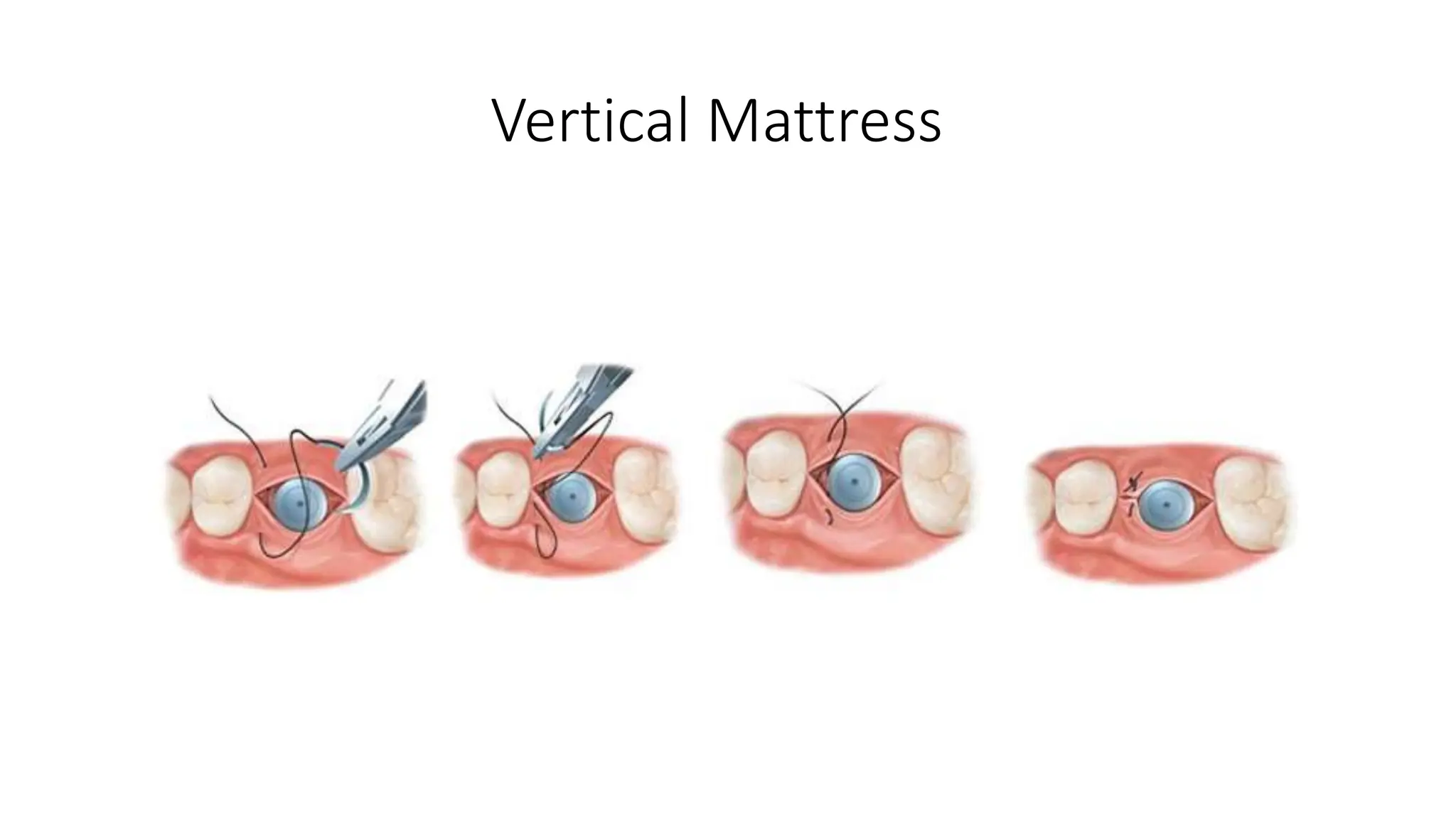
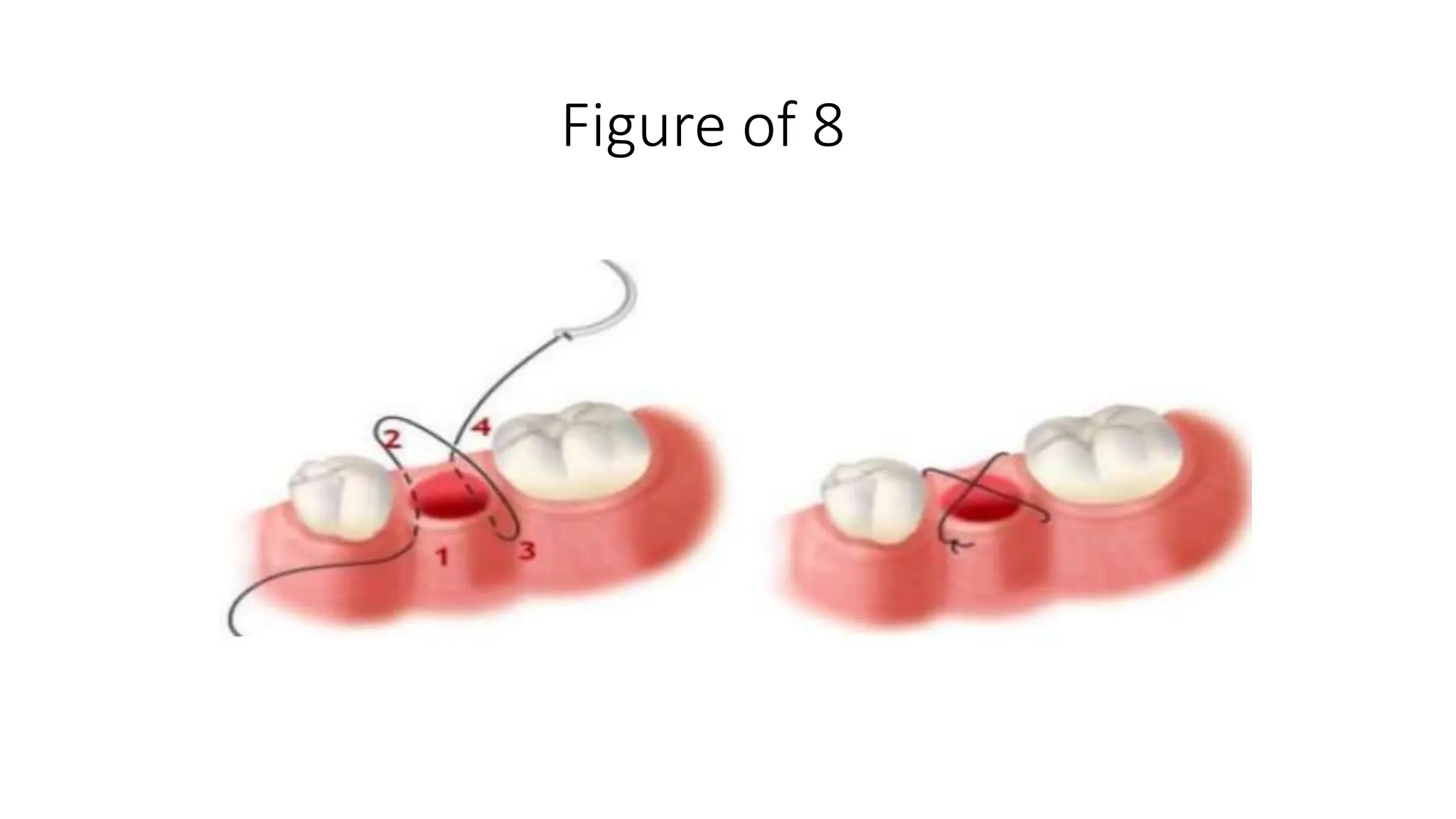
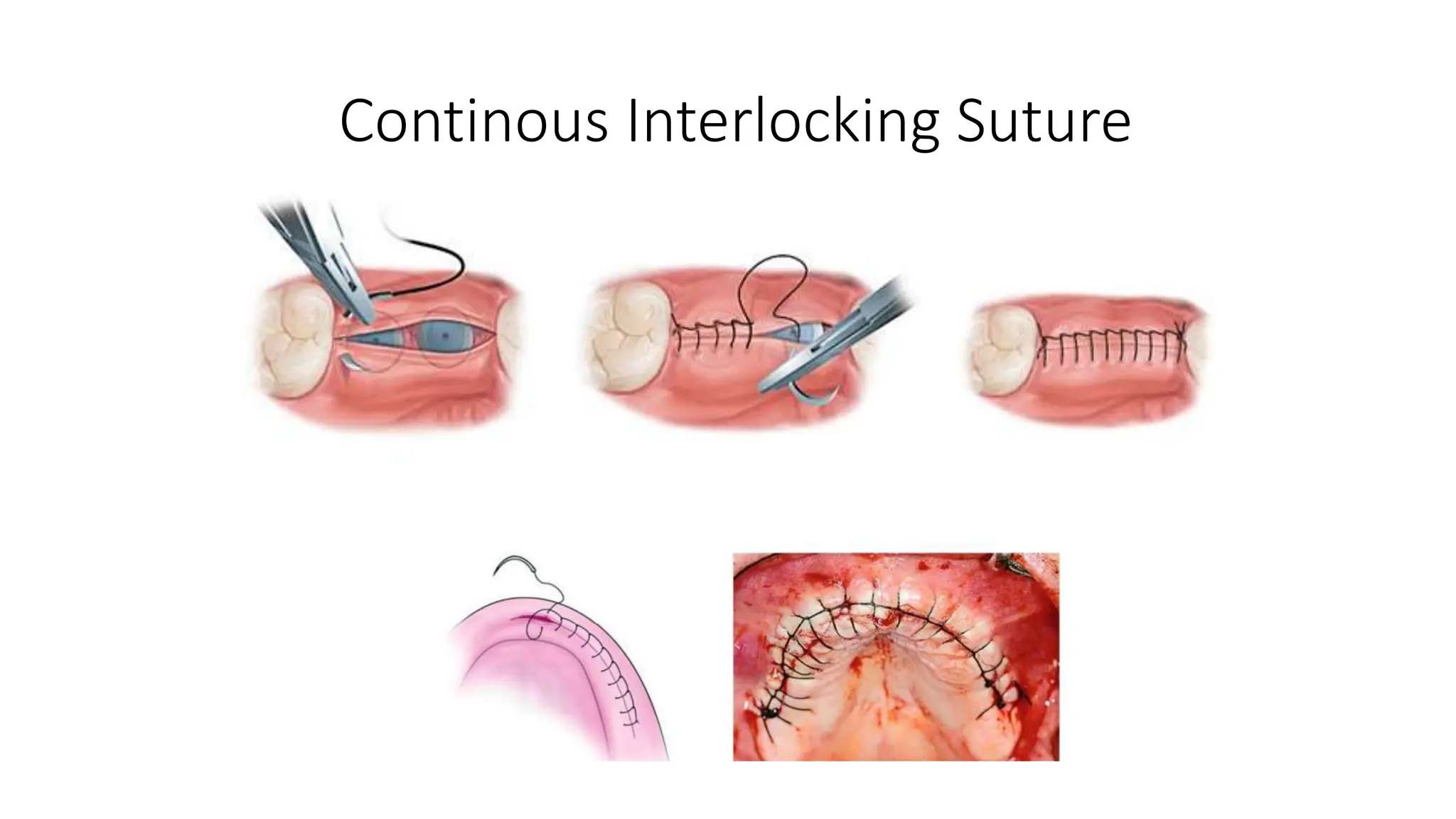
- Types of sutures and knots like interrupted, mattress, figure-of-8, and how to tie square and surgeon's knots.
- Factors for successful osseointegration of dental implants like using titanium materials, preventing contamination and infection at the implantation site, using coolant during drilling, and delayed loading to allow for osseointegr