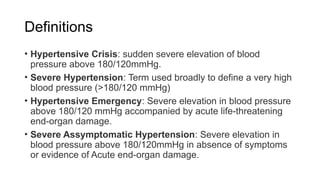
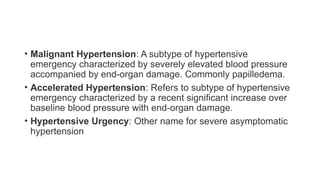
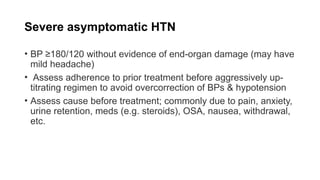
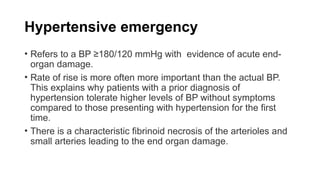
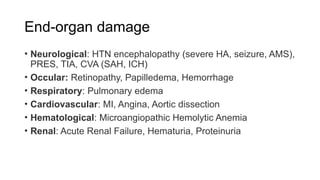
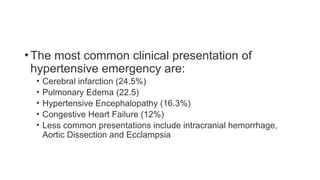
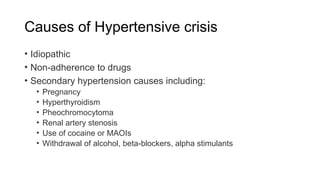
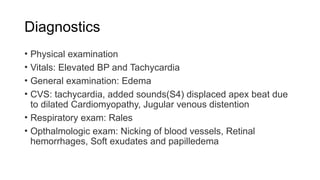
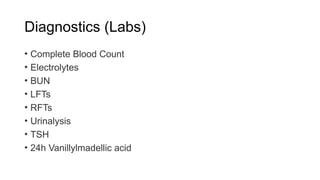
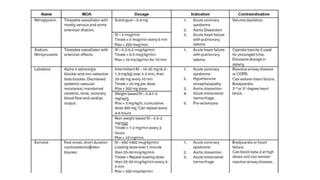
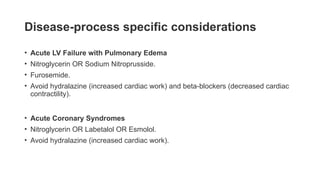
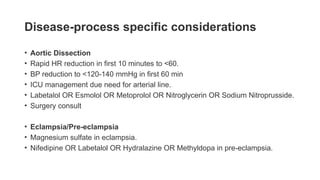
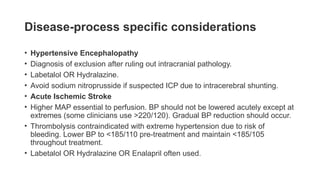
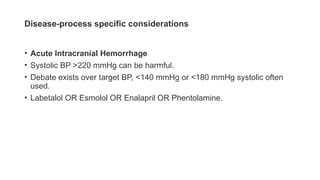
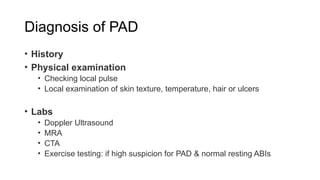
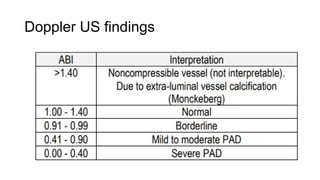
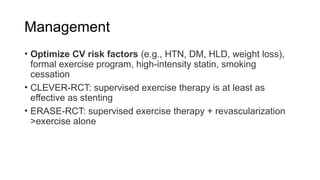
The document provides a comprehensive overview of hypertensive crises and peripheral arterial diseases, detailing definitions, causes, diagnostics, and management strategies. It describes various conditions associated with elevated blood pressure, such as hypertensive emergencies and severe asymptomatic hypertension, as well as risk factors and symptoms of peripheral artery disease. The management section emphasizes the importance of individualized treatment plans and monitoring, along with specific considerations for acute conditions.