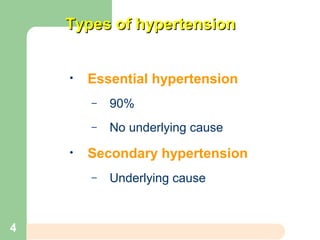
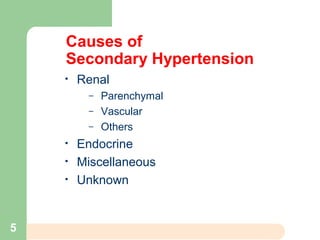
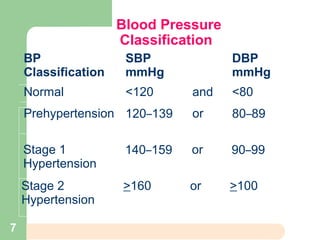
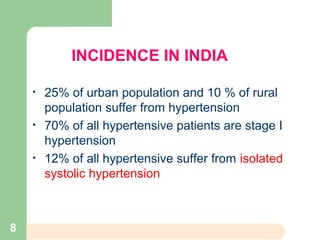
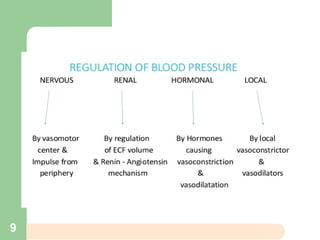
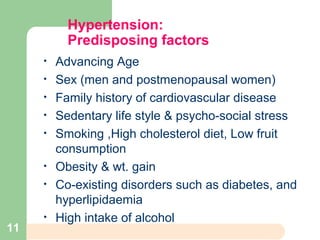
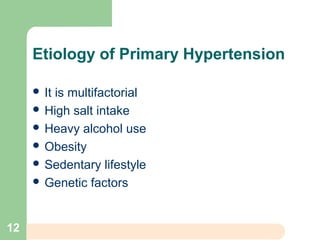
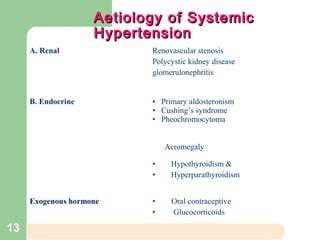
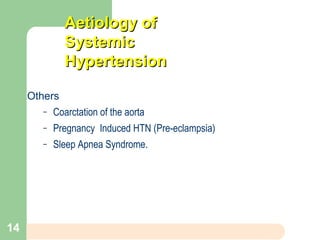
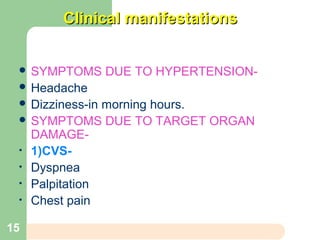
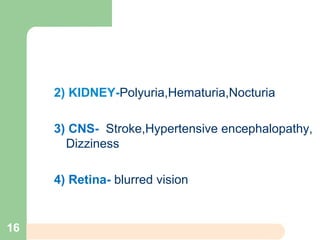
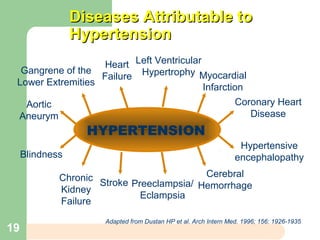
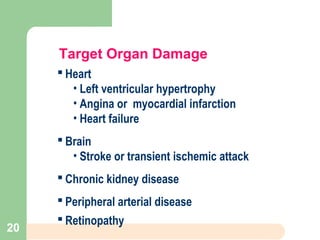
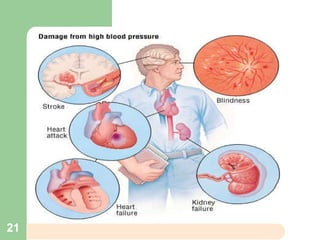
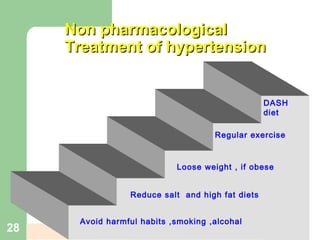
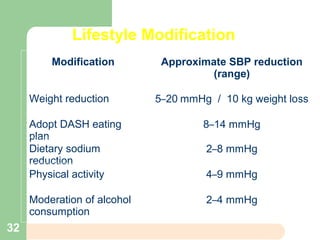
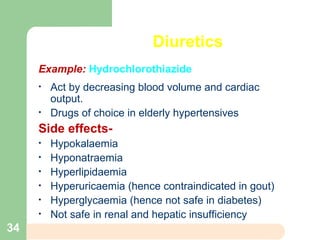
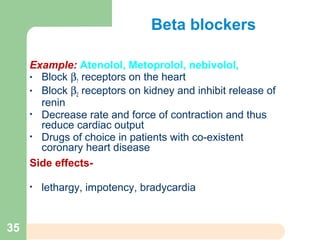
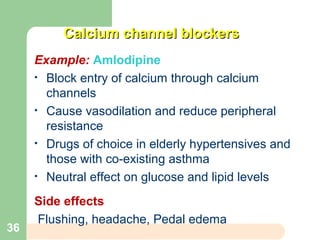
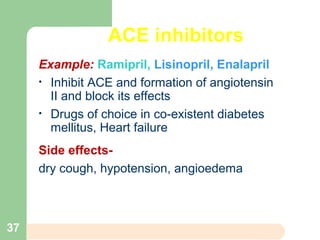
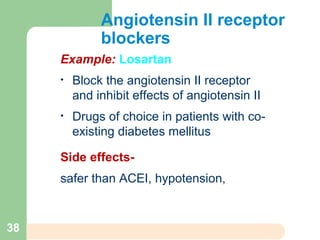
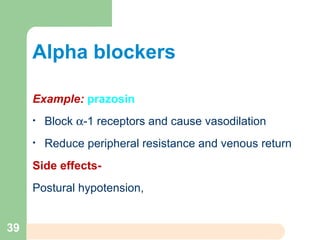
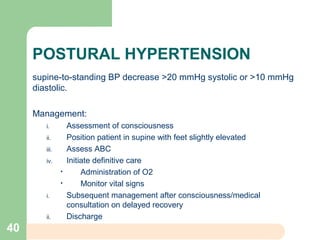
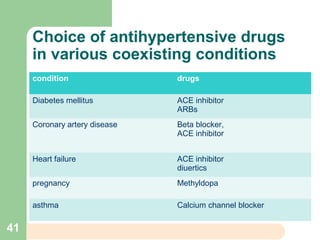
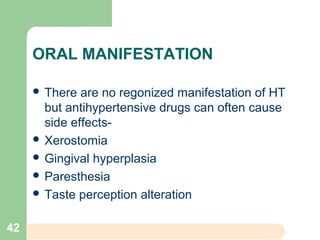
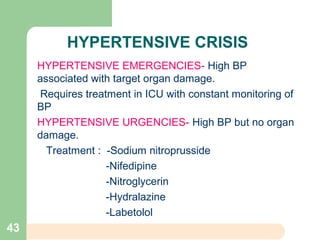
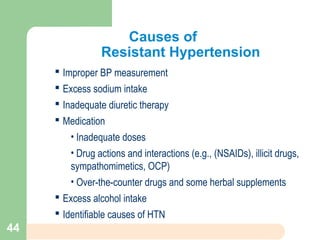
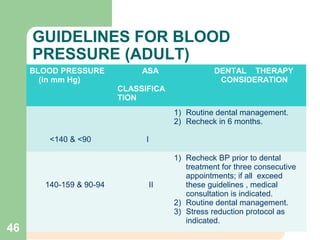
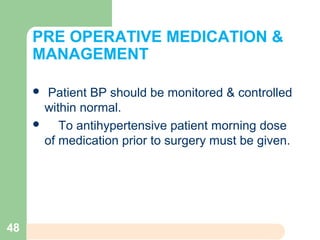
This document summarizes a presentation on hypertension given by Aanshika Tiwari. It defines hypertension as a blood pressure above 140/90 mmHg. It describes the types, causes, risk factors, signs and symptoms, diagnosis, and treatment of hypertension. Regarding treatment, it discusses both non-pharmacological options like lifestyle modifications as well as various classes of antihypertensive drugs. It also addresses hypertension management in dentistry.