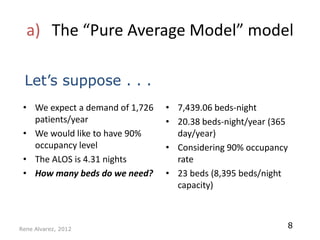
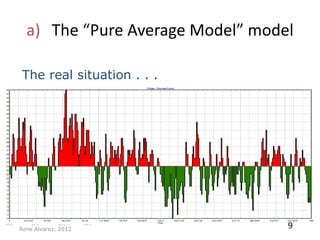
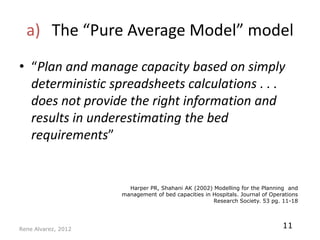
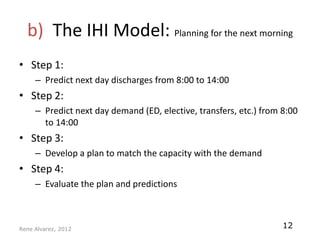
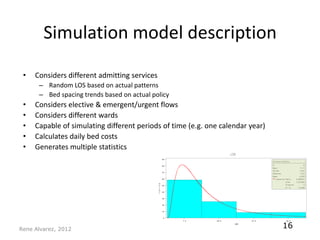
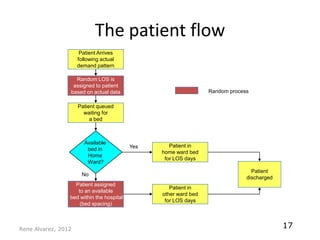
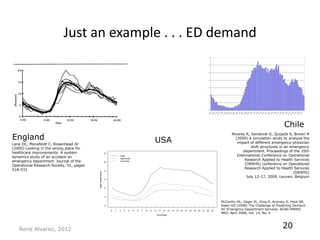
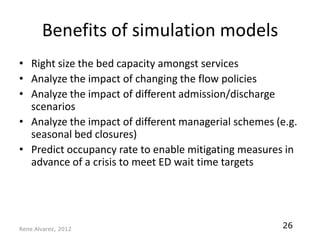
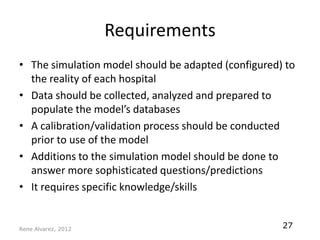
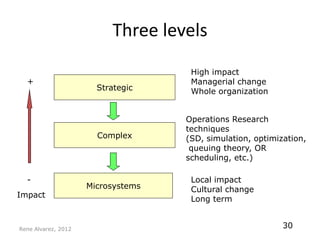
This document discusses hospital capacity management and different models used. It proposes a more comprehensive simulation model that considers random patient lengths of stay, bed availability, and patient flows to better predict capacity needs. Such a model could improve long and medium-term planning by predicting occupancy levels and evaluating different scenarios. Building an accurate simulation model requires collecting and analyzing hospital-specific data.