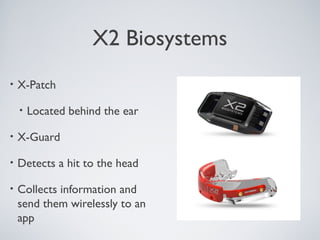
This document discusses sports-related concussions, including what they are, their effects on brain function, signs and symptoms, potential long-term issues like chronic traumatic encephalopathy, diagnostic testing methods, return-to-play protocols, and new technologies to improve safety and monitoring. A concussion is a traumatic brain injury caused by a blow to the head that results in rapid head movement. This can disrupt normal brain cell function and lead to issues with thinking, memory, and balance. Repeated concussions may cause a progressive brain disease called chronic traumatic encephalopathy. Baseline testing, SCAT tests, and impact tests help evaluate and monitor concussion recovery. Strict return-to-play guidelines aim to prevent second-impact