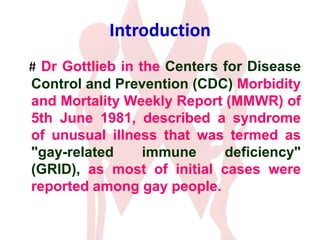
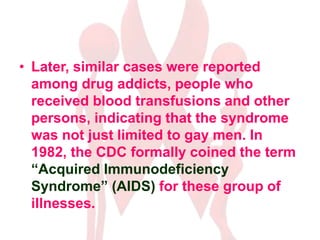
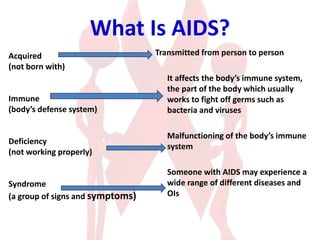
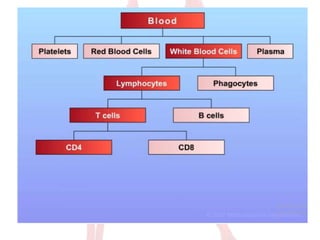
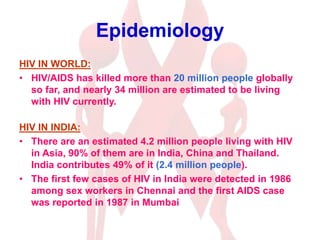
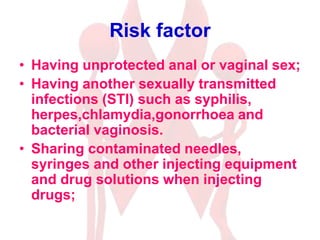
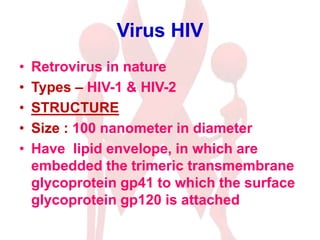
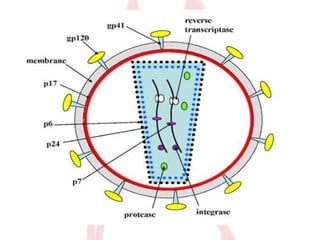
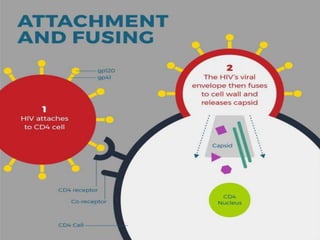
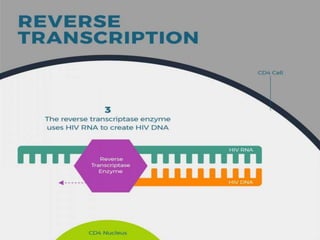
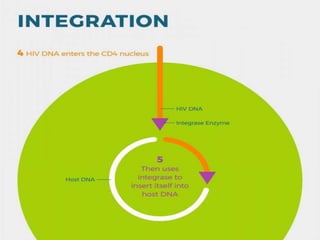
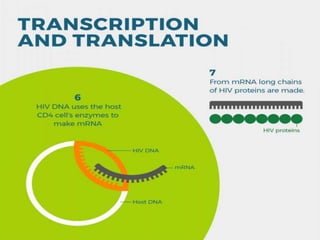
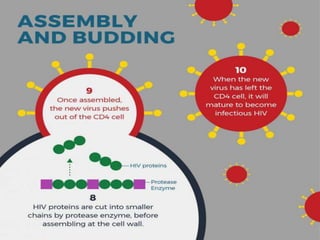
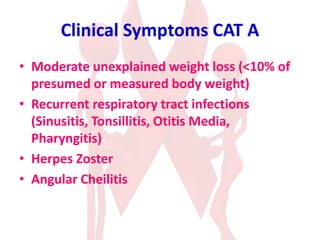
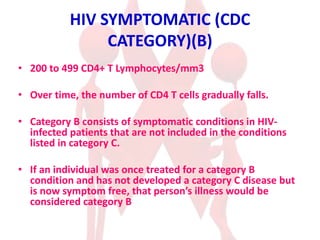
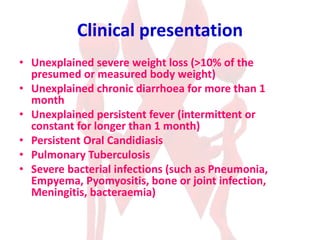
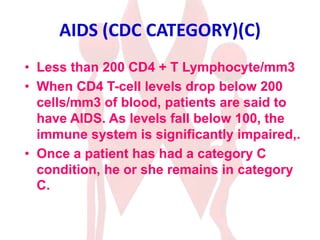
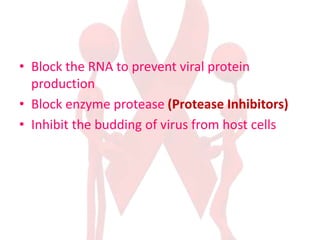
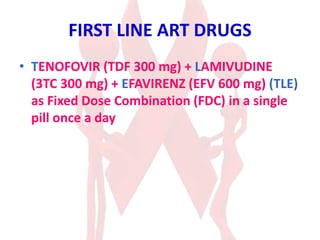
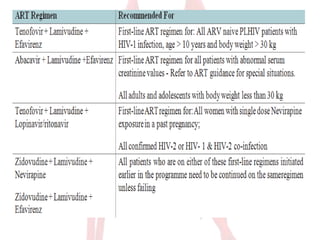
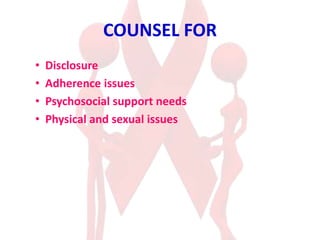
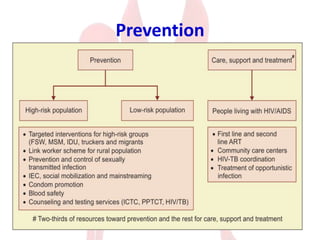
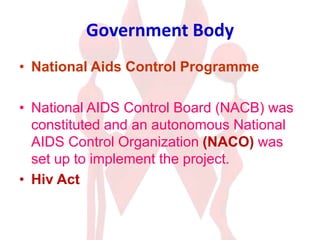
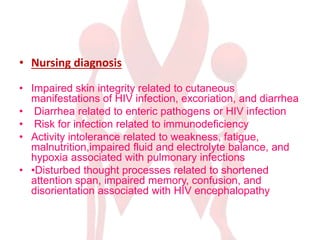
HIV/AIDS seminar covered the history, epidemiology, transmission, stages, diagnosis and treatment of HIV/AIDS. It discussed how HIV attacks and destroys CD4 cells. Diagnosis involves antibody and viral load tests. Treatment goals are to suppress the virus with antiretroviral therapy (ART) using three drug combinations. Nursing care focuses on managing symptoms, preventing infections, treatment adherence and palliative care.