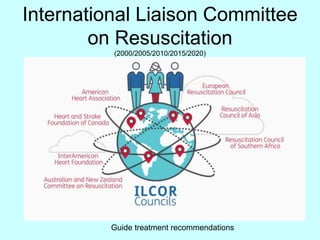
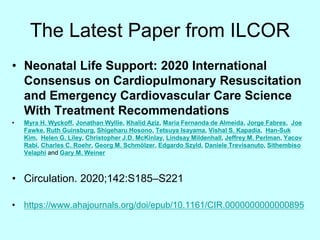
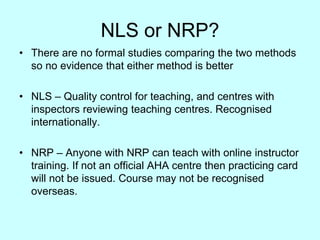
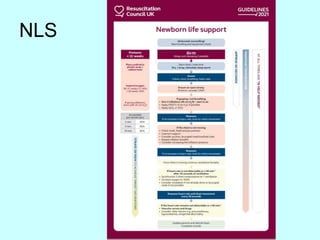
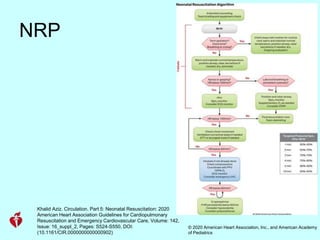
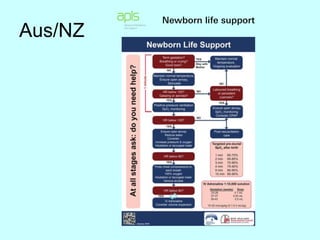
This document discusses changes in delivery room practices for newborn infants around the world based on guidelines from the International Liaison Committee on Resuscitation (ILCOR). Key points discussed include:
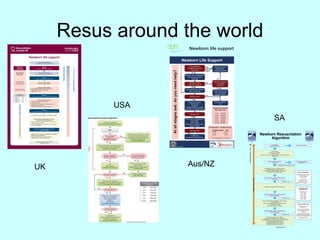
- ILCOR provides treatment recommendations that guide resuscitation protocols worldwide.
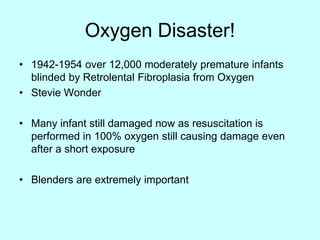
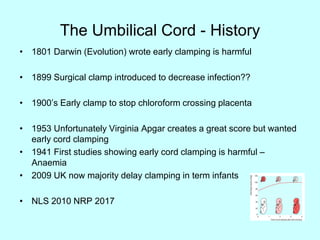
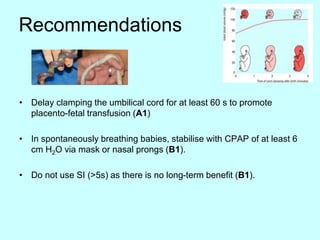
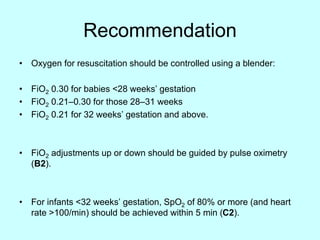
- Practices vary between regions but are converging based on ILCOR guidelines, including delayed umbilical cord clamping, use of CPAP, and tight control of oxygen levels.
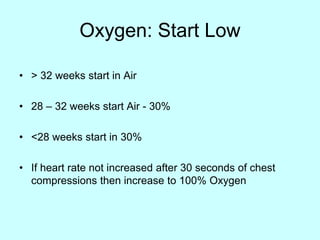
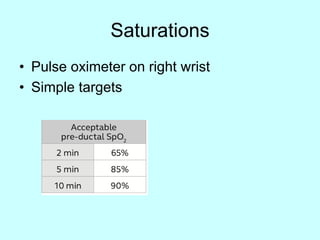
- Recent guidelines recommend delaying umbilical cord clamping for at least 60 seconds, use of CPAP for stabilizing breathing in preterm infants, and controlling oxygen levels using a blender to avoid hyperoxia.