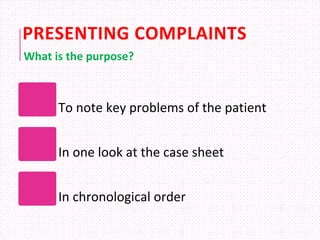
1. History taking provides vital information to arrive at a diagnosis in over 70% of cases by allowing the patient to describe their illness and systematically inquiring about their medical history, presenting complaints, past illnesses, habits, and family history.
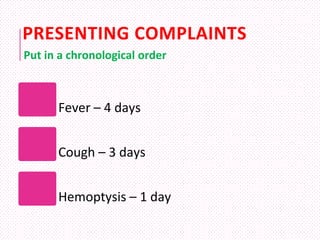
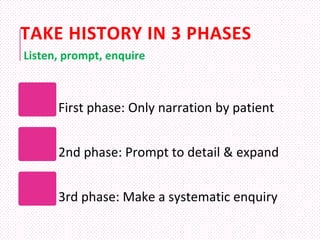
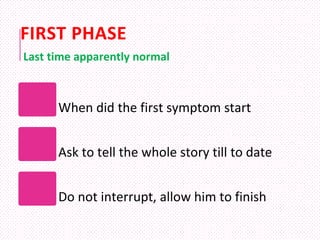
2. It is important to build rapport with the patient, have them describe their illness chronologically without interruption, then prompt them for details in key areas before making a systematic inquiry about each body system.
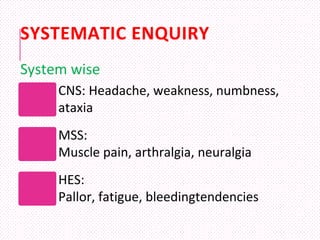
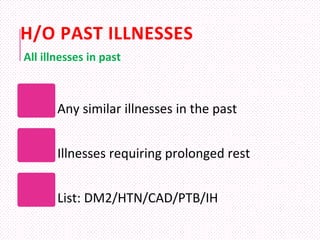
3. A thorough history should explore the patient's presenting complaints, history of present illness, investigation and treatment details, past medical history, personal history, and family history in order to understand how their illness started and progressed and arrive at the most likely diagnostic possibilities based on