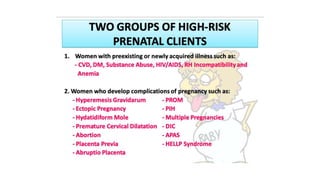
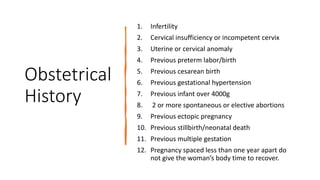
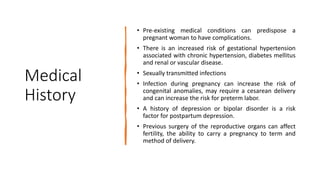
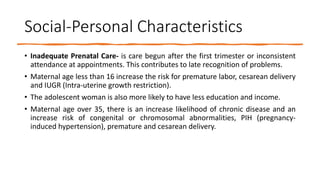
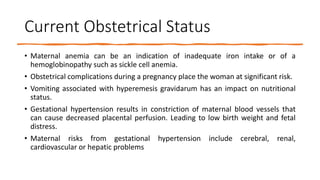
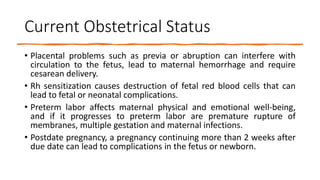
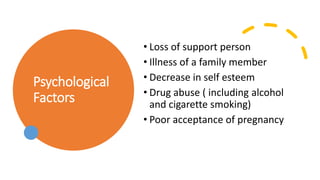
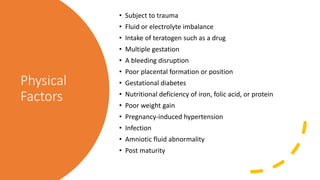
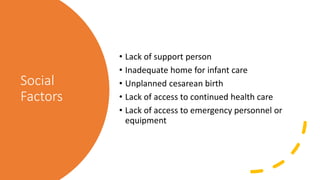
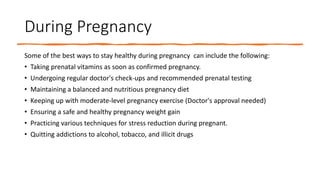
This document discusses care of at-risk and high-risk mothers and children. It defines a high-risk pregnancy as one where a medical condition, complication, or external factor jeopardizes the health of the mother or fetus. Factors that can contribute to high-risk pregnancies include obstetric history, medical history, current pregnancy status, and social factors. The document outlines various psychological, social, and physical risk factors during the pre-pregnancy, pregnancy, labor/birth stages. It emphasizes the importance of prevention through preconception care and management during pregnancy through frequent monitoring and specialized care.