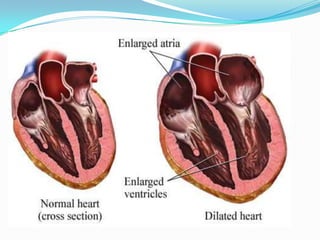
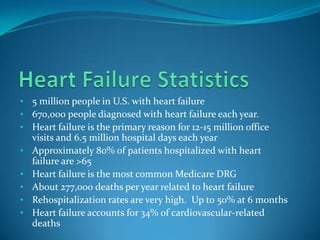
Heart failure is a complex syndrome where the heart cannot properly fill with or pump blood, resulting from structural or functional cardiac issues. It affects over 5 million Americans and is a leading cause of hospitalization. Mortality rates following hospitalization are 10.4% at 30 days and increase to 42.3% at 5 years. Symptoms include dyspnea, fatigue, edema and more. Causes include coronary artery disease, hypertension, cardiomyopathy and others. Diagnosis involves labs, imaging like echocardiogram and ischemic evaluation. Treatment ranges from lifestyle changes to advanced devices and transplantation.