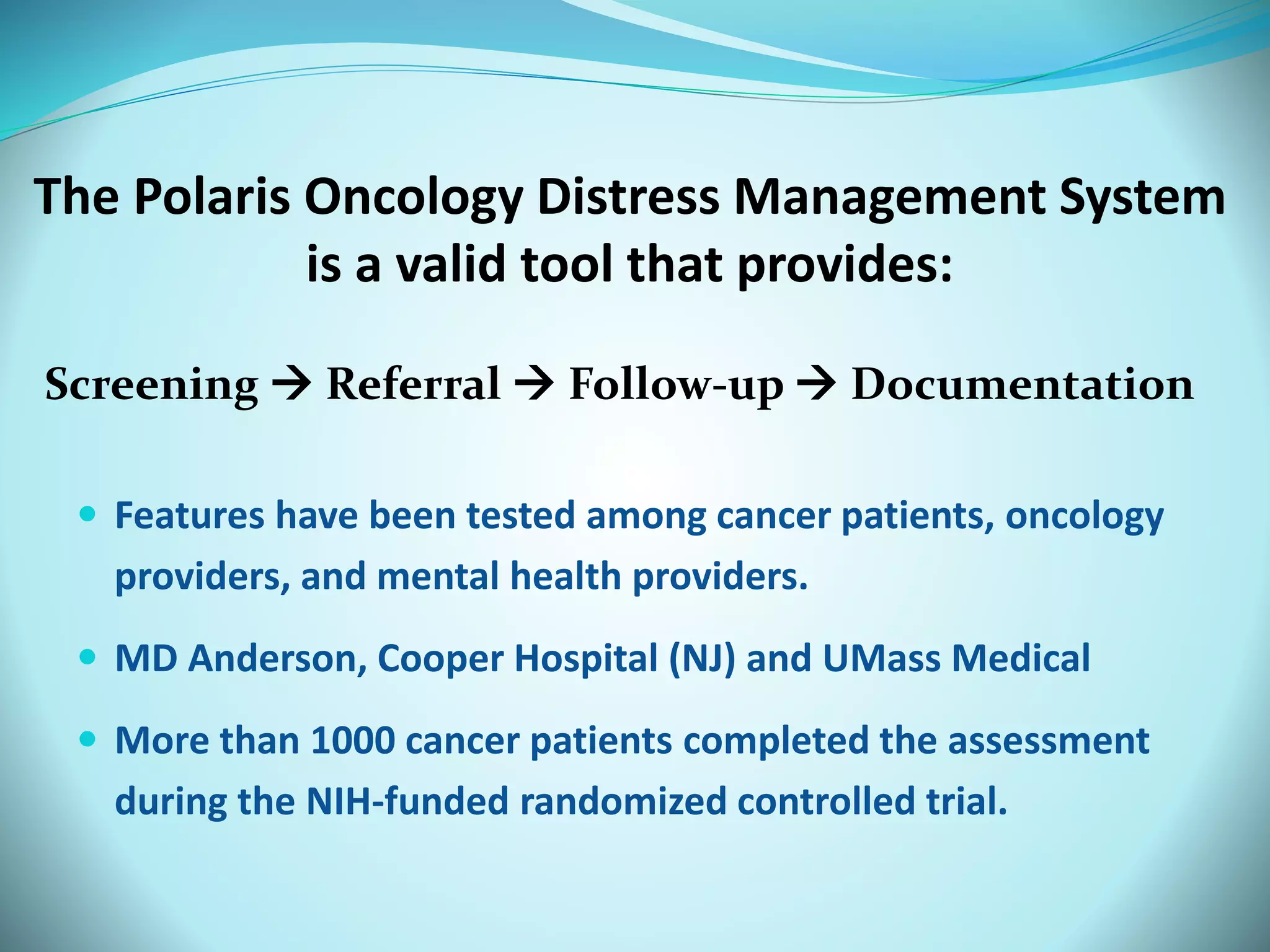
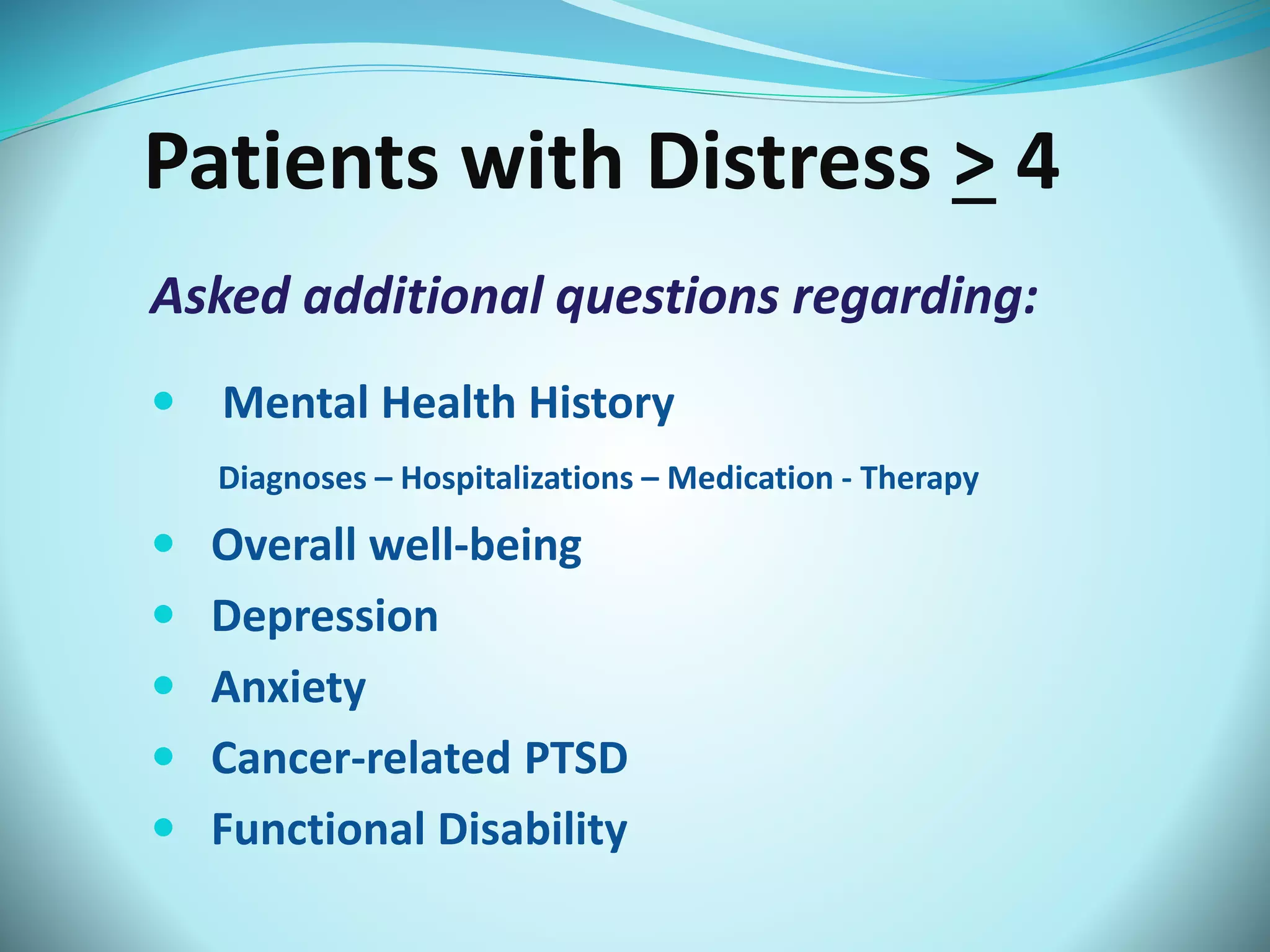
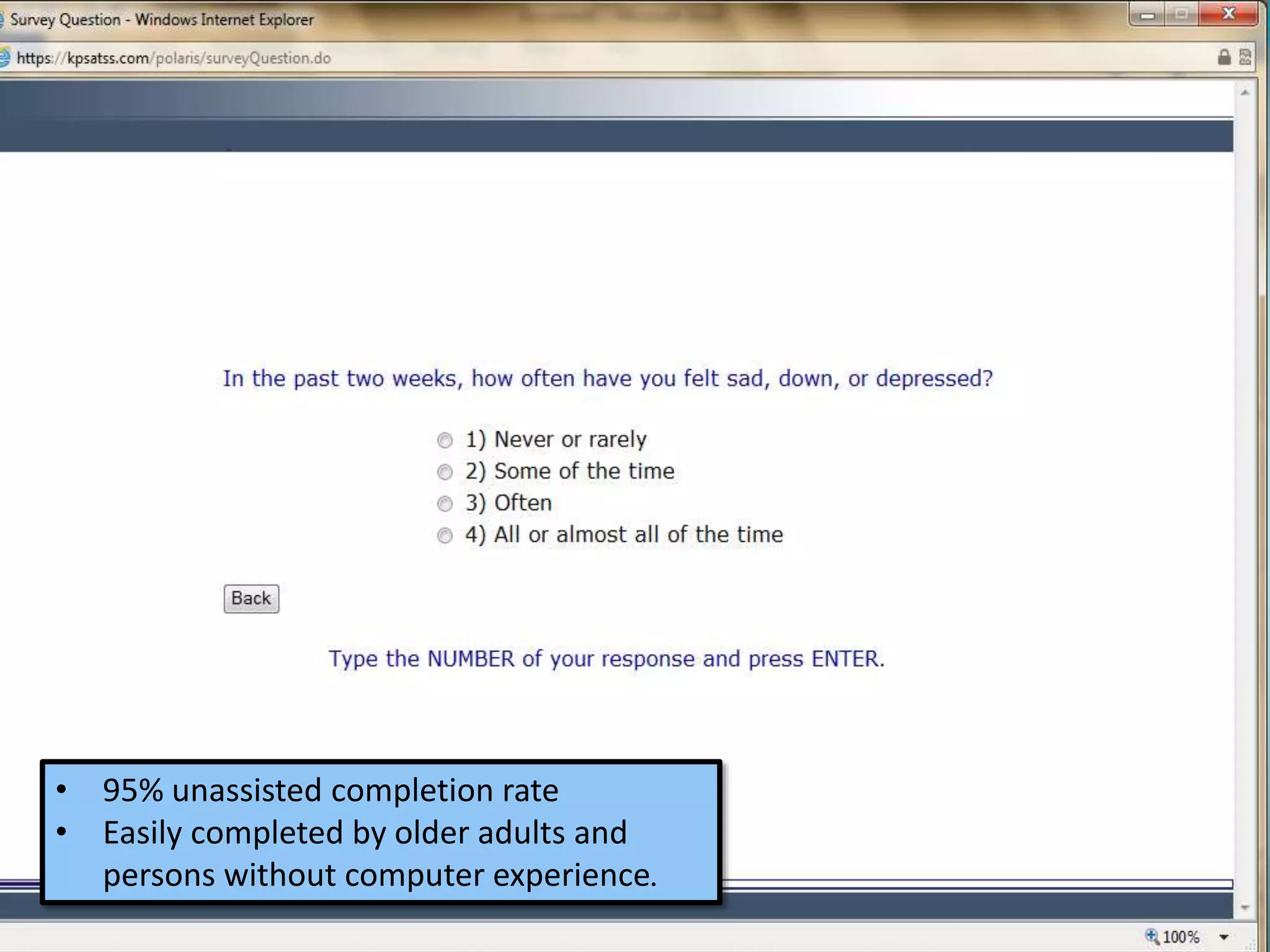
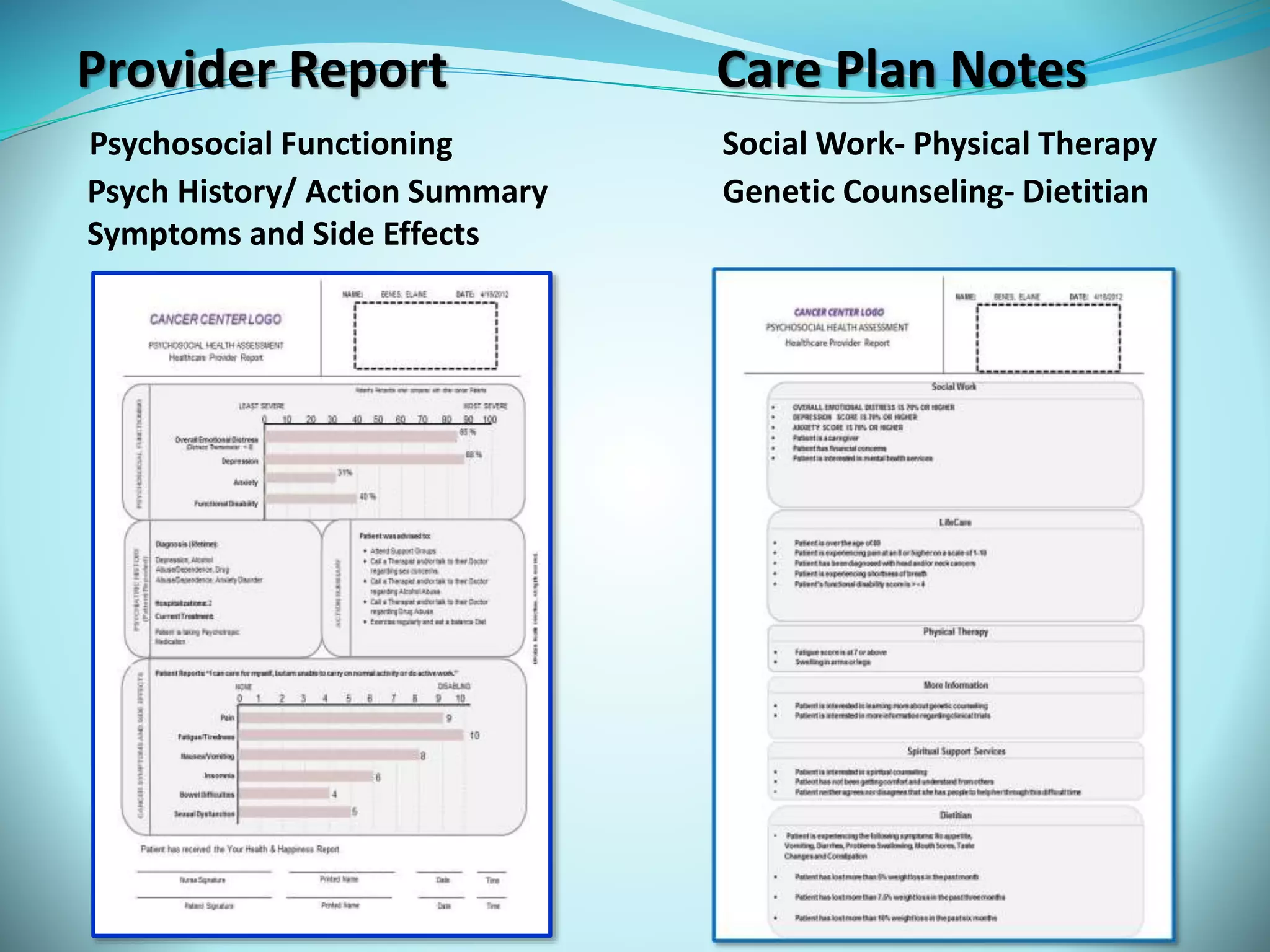
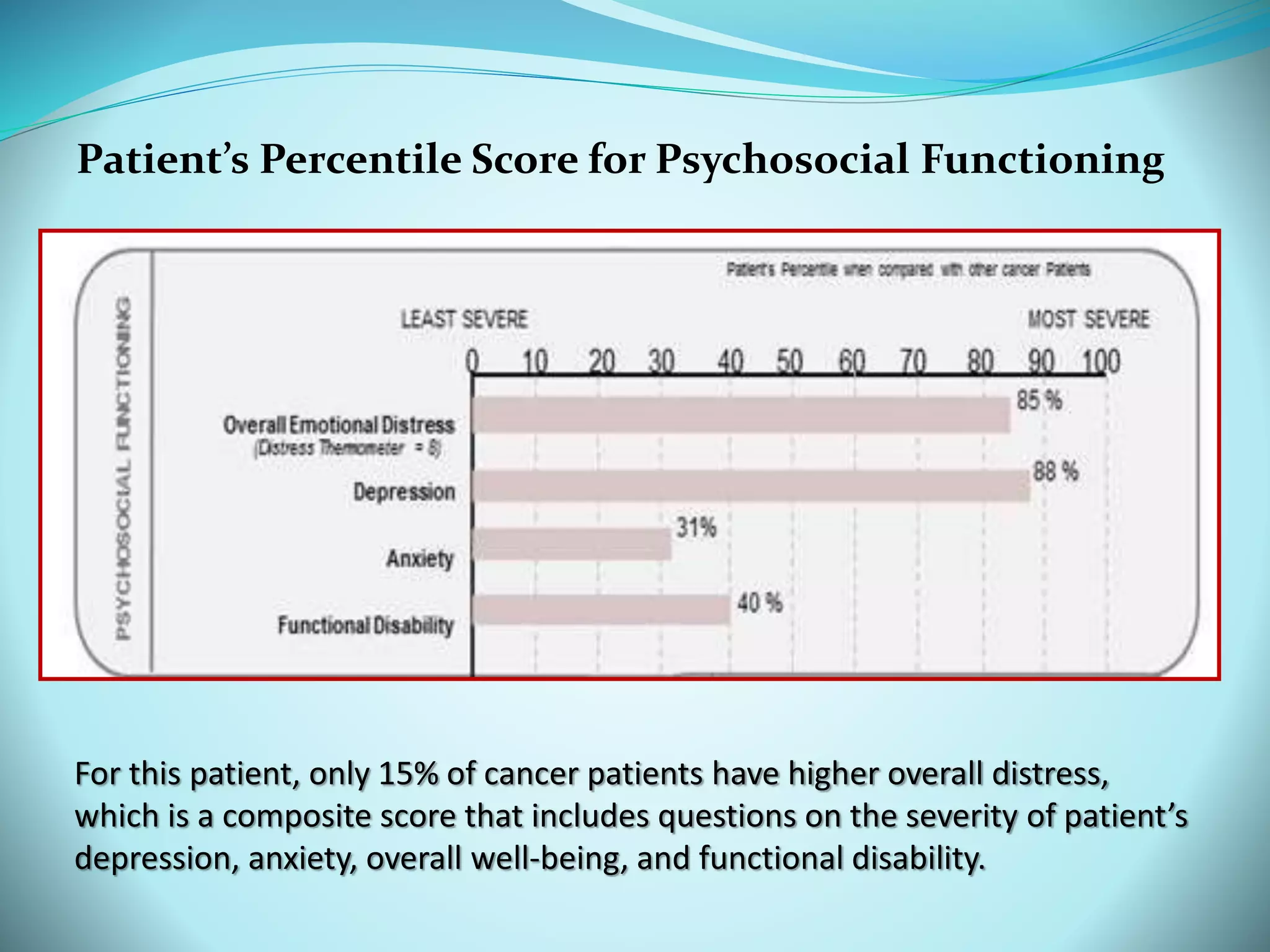
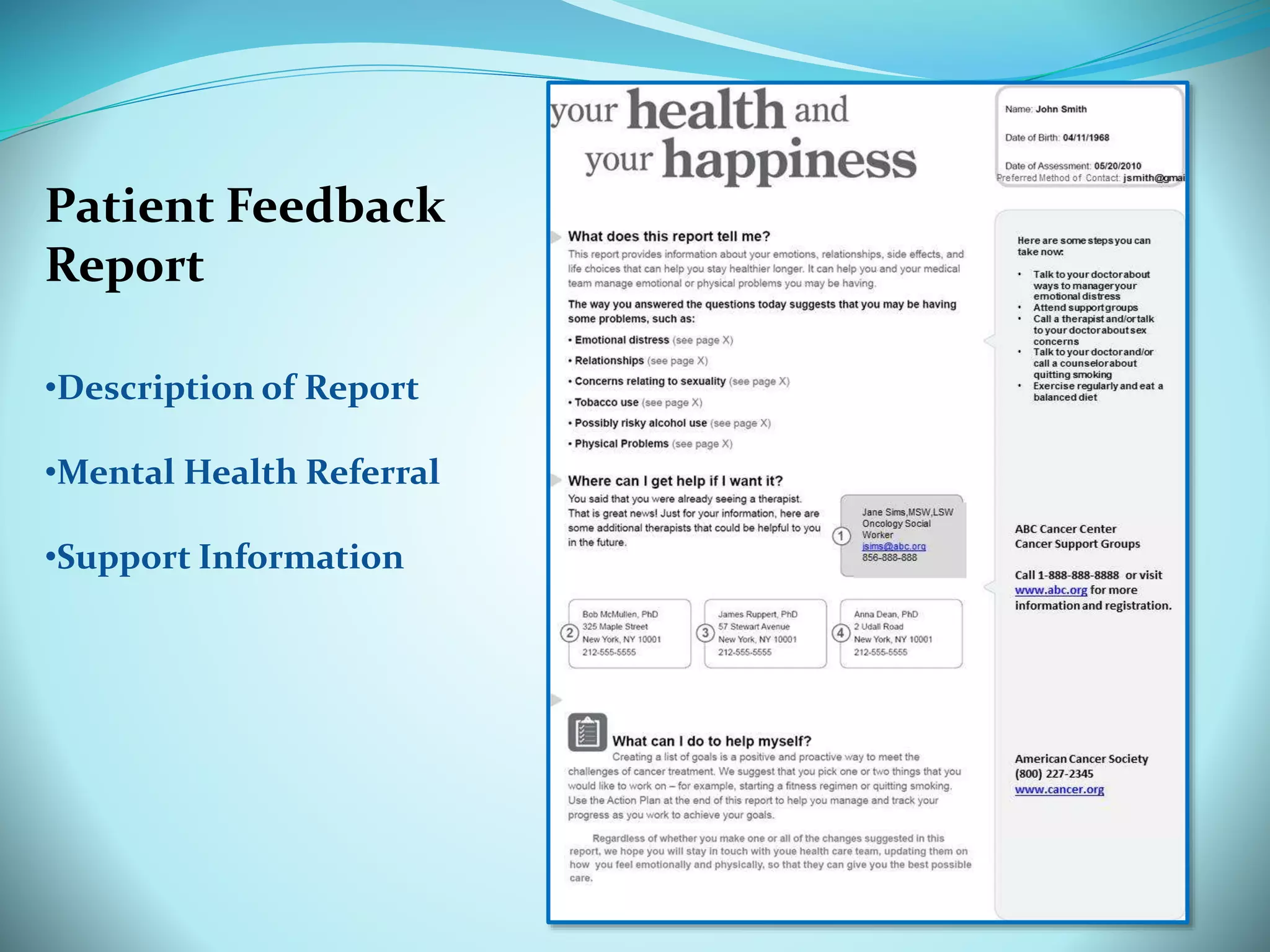
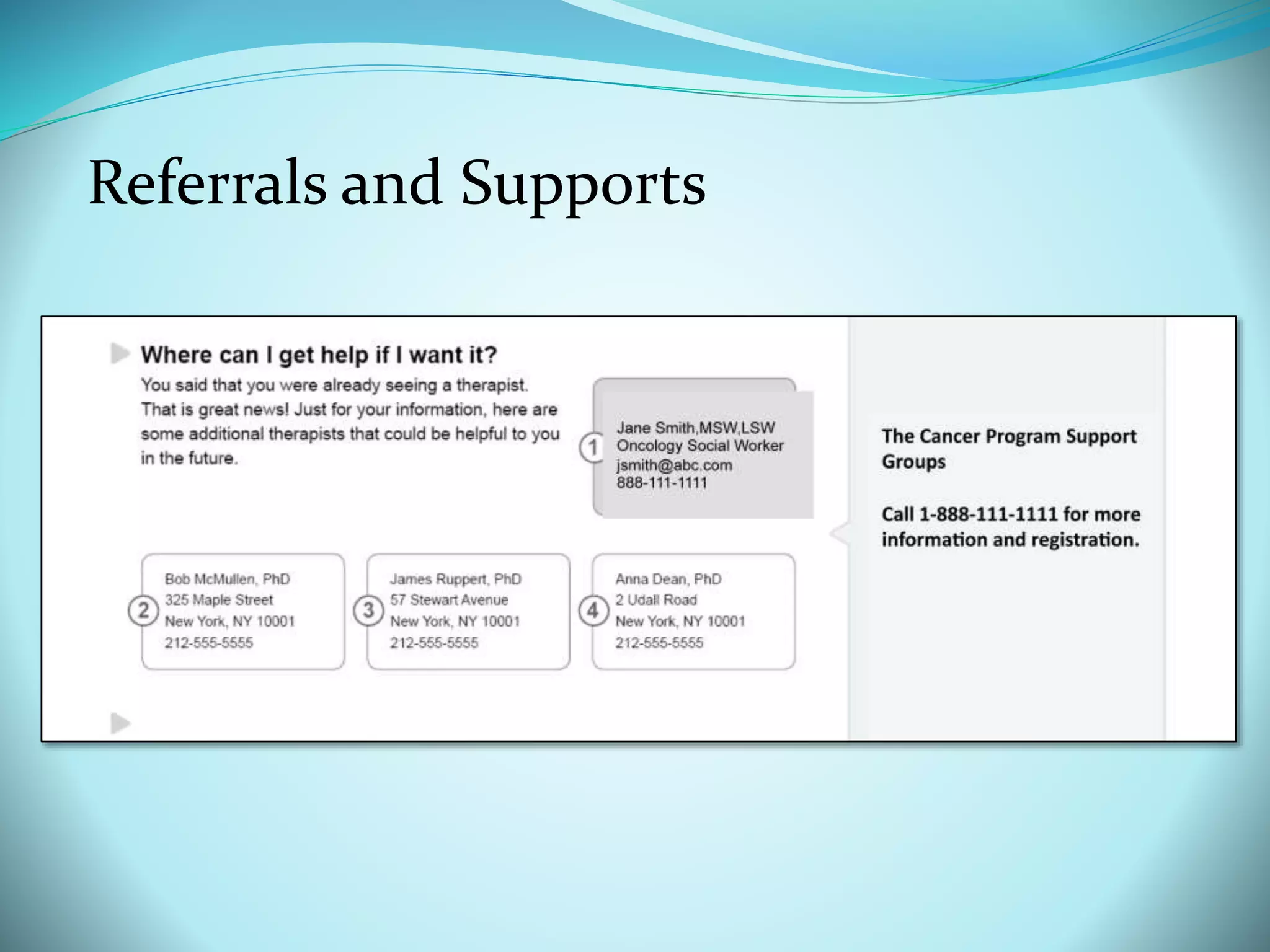
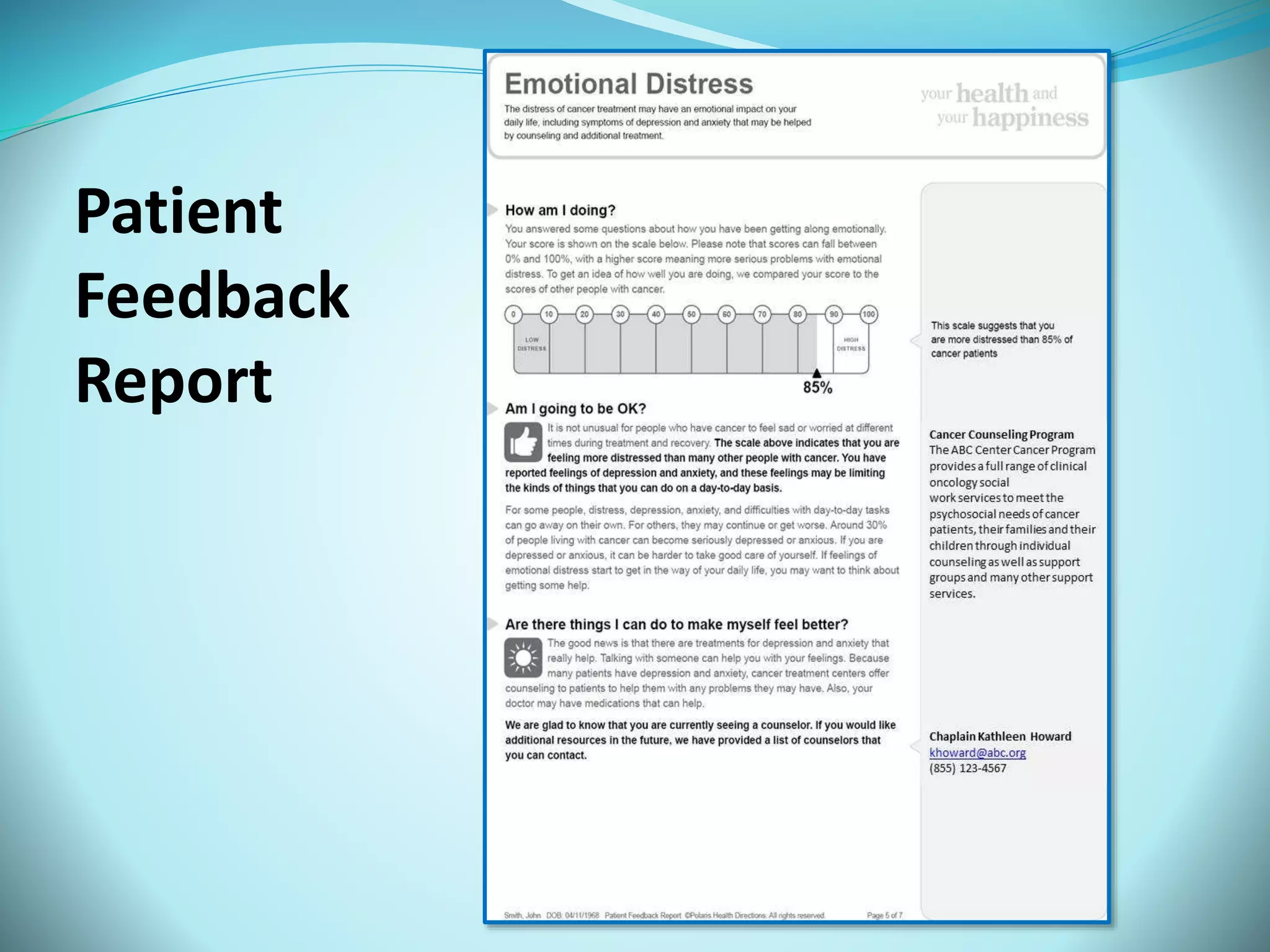
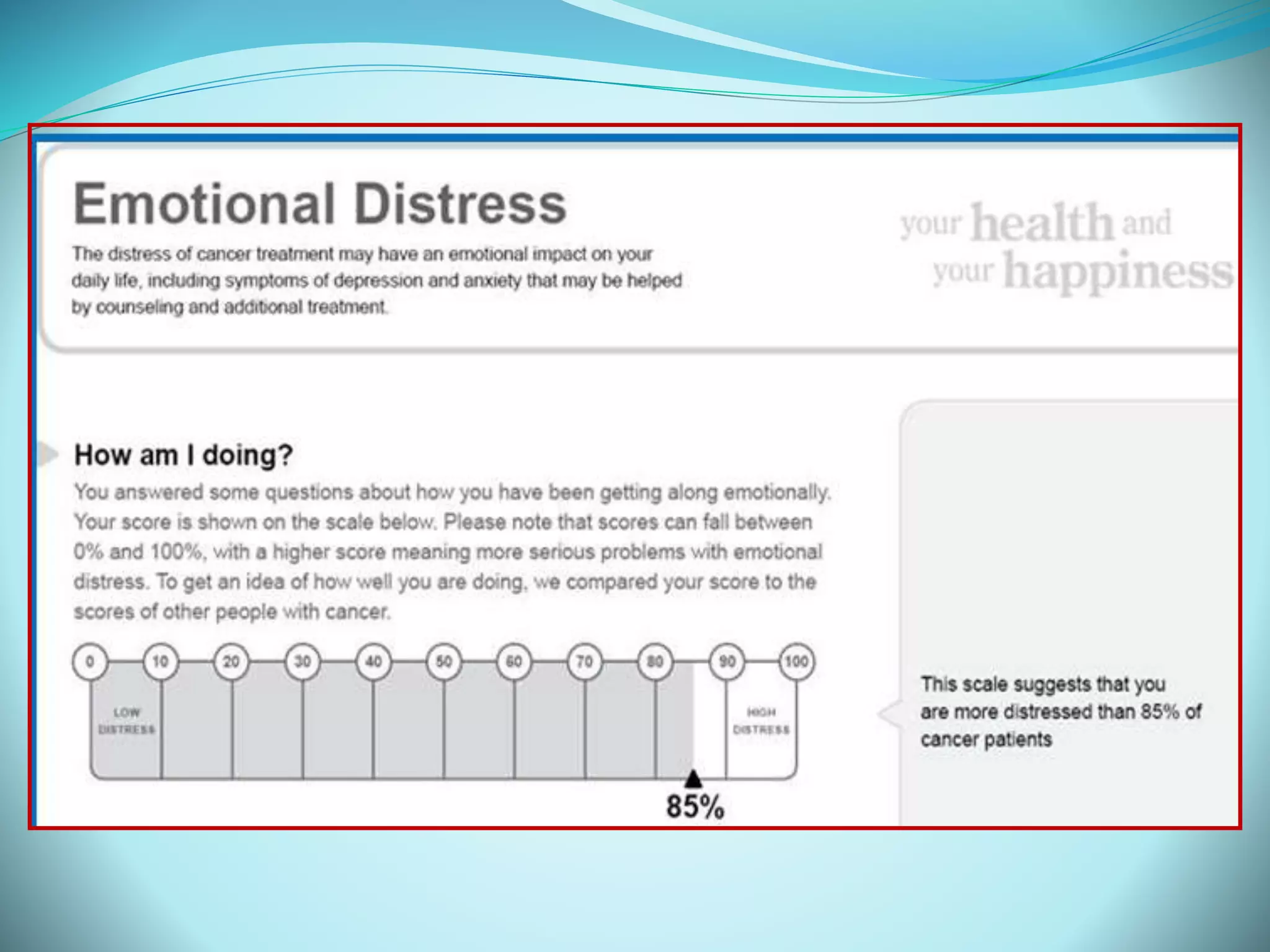
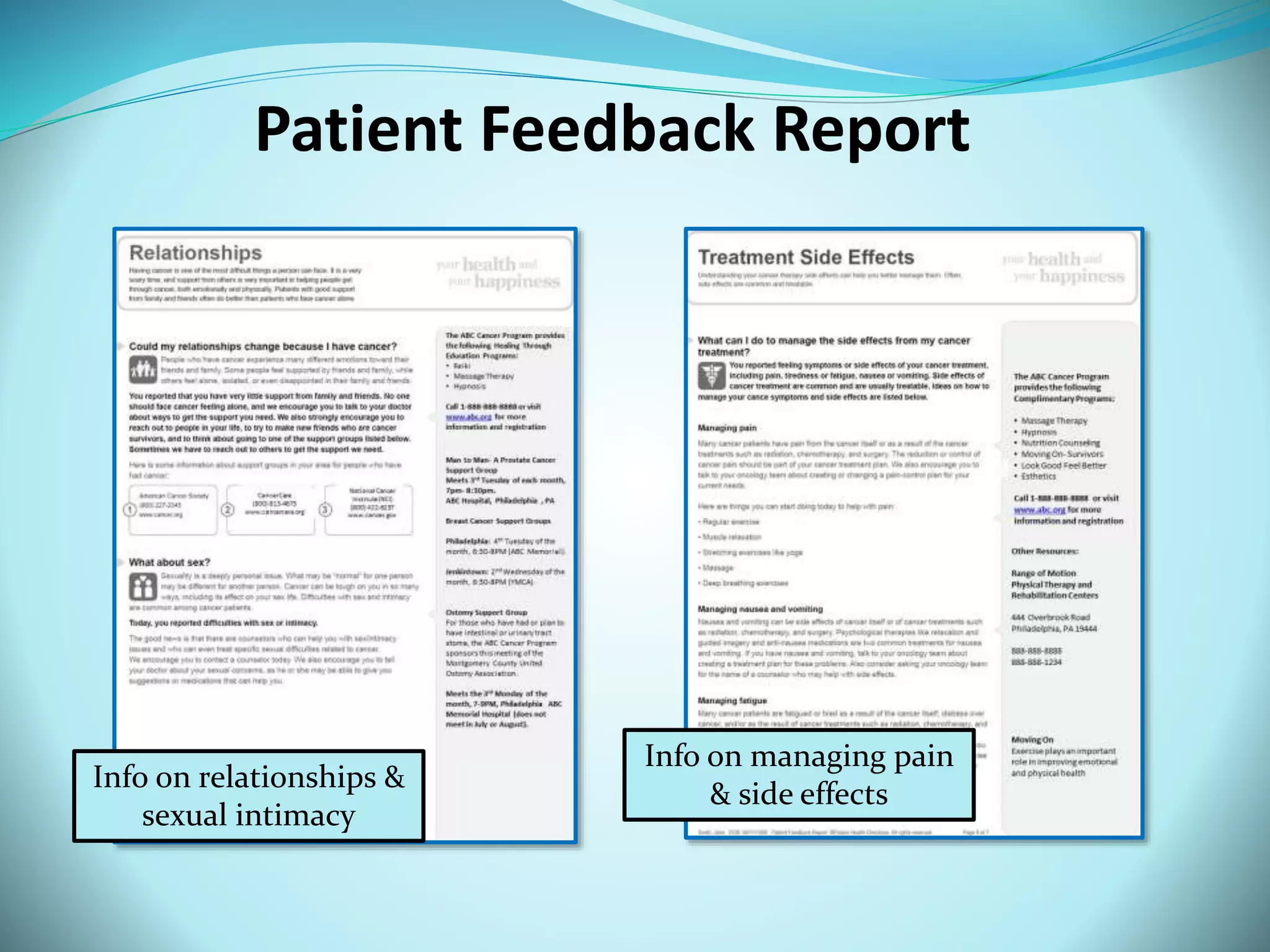
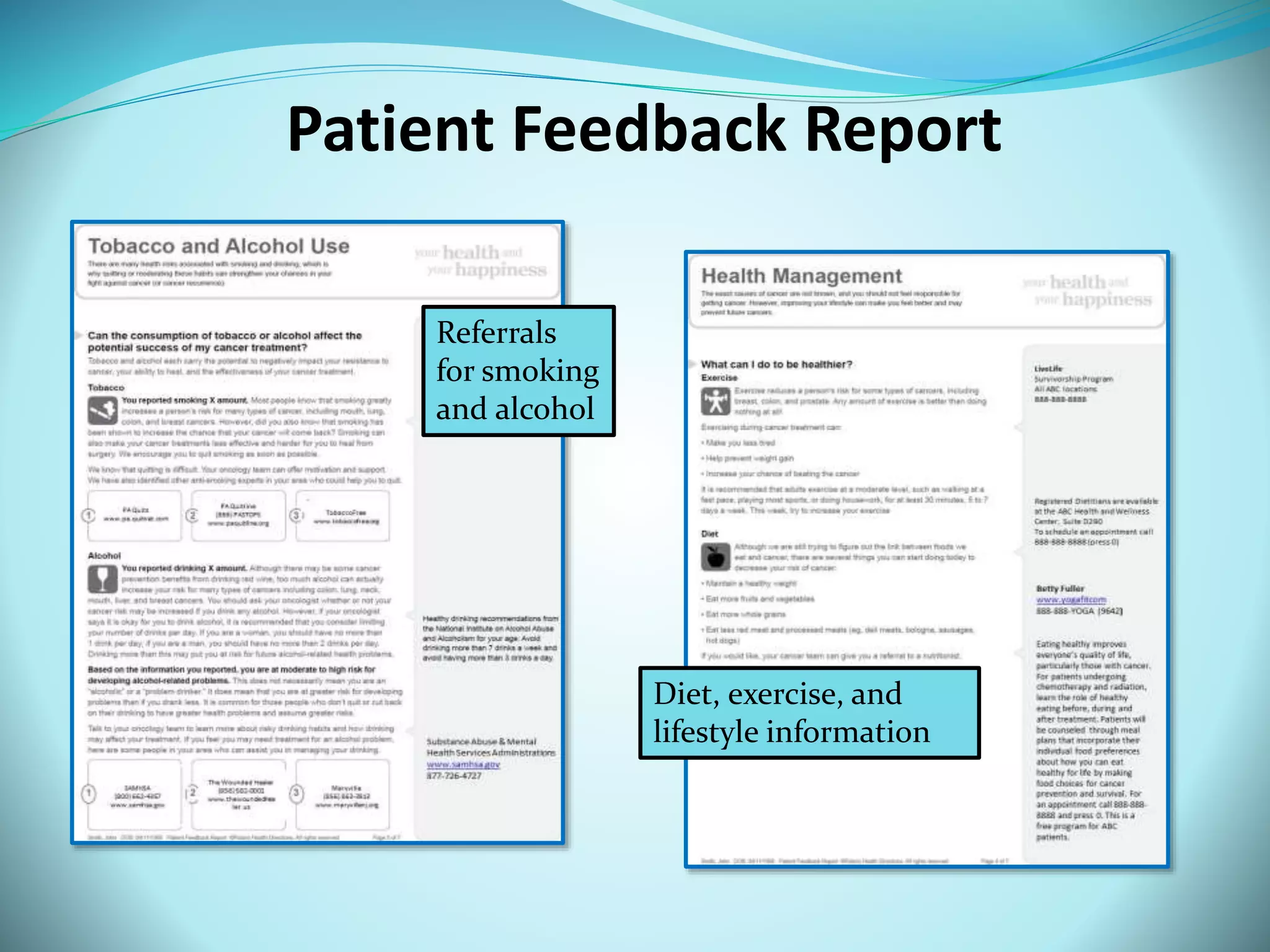
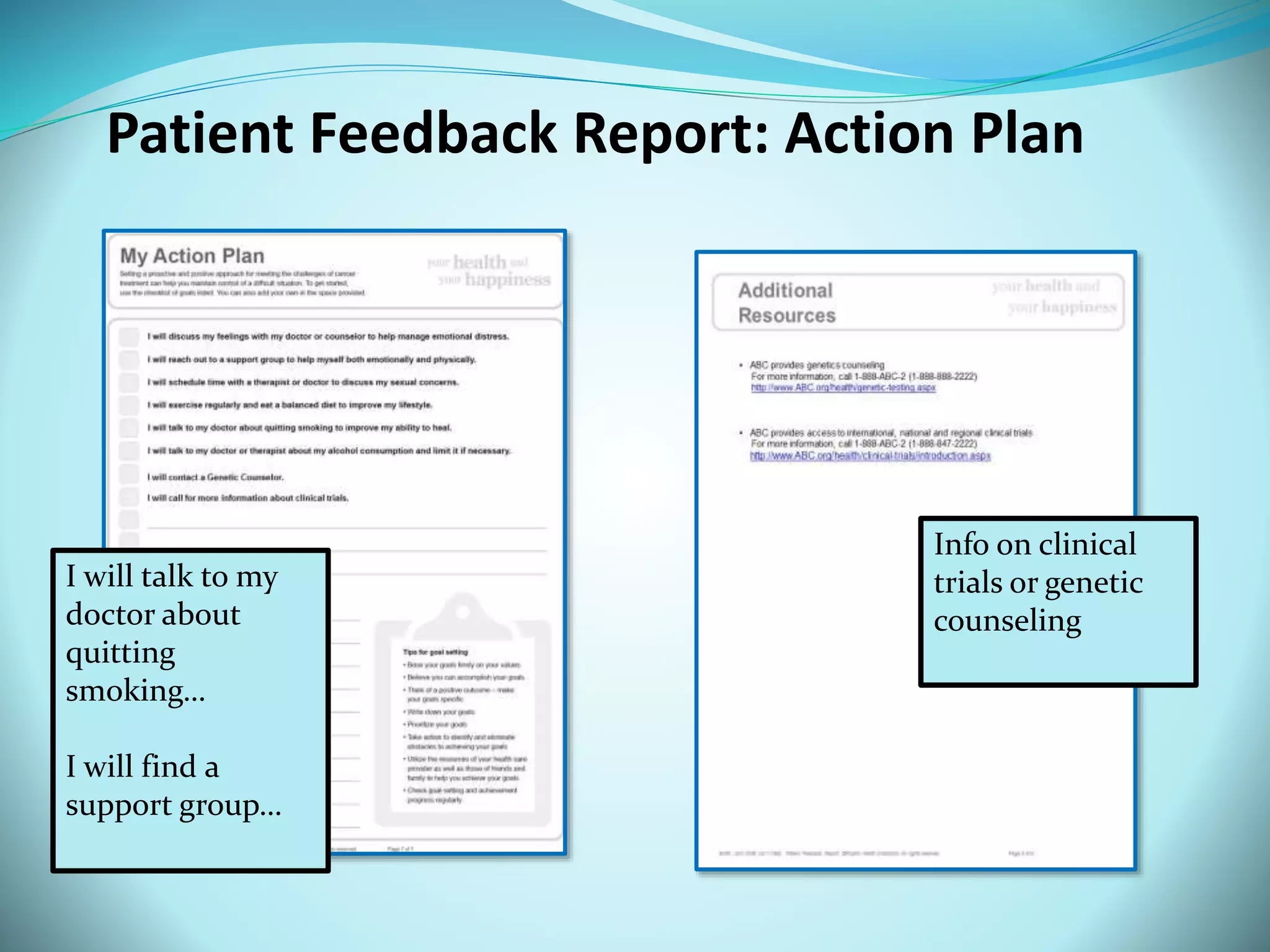
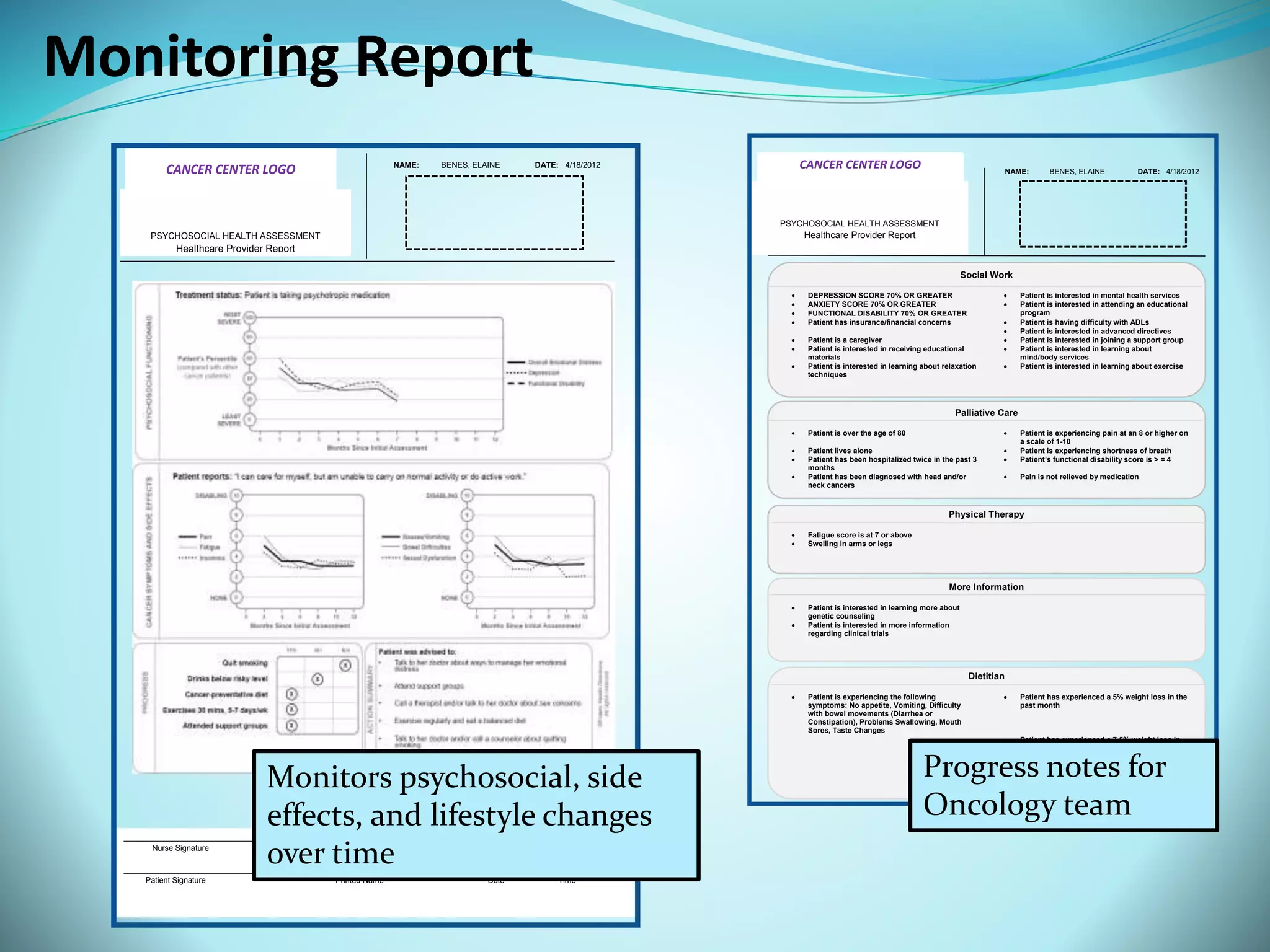
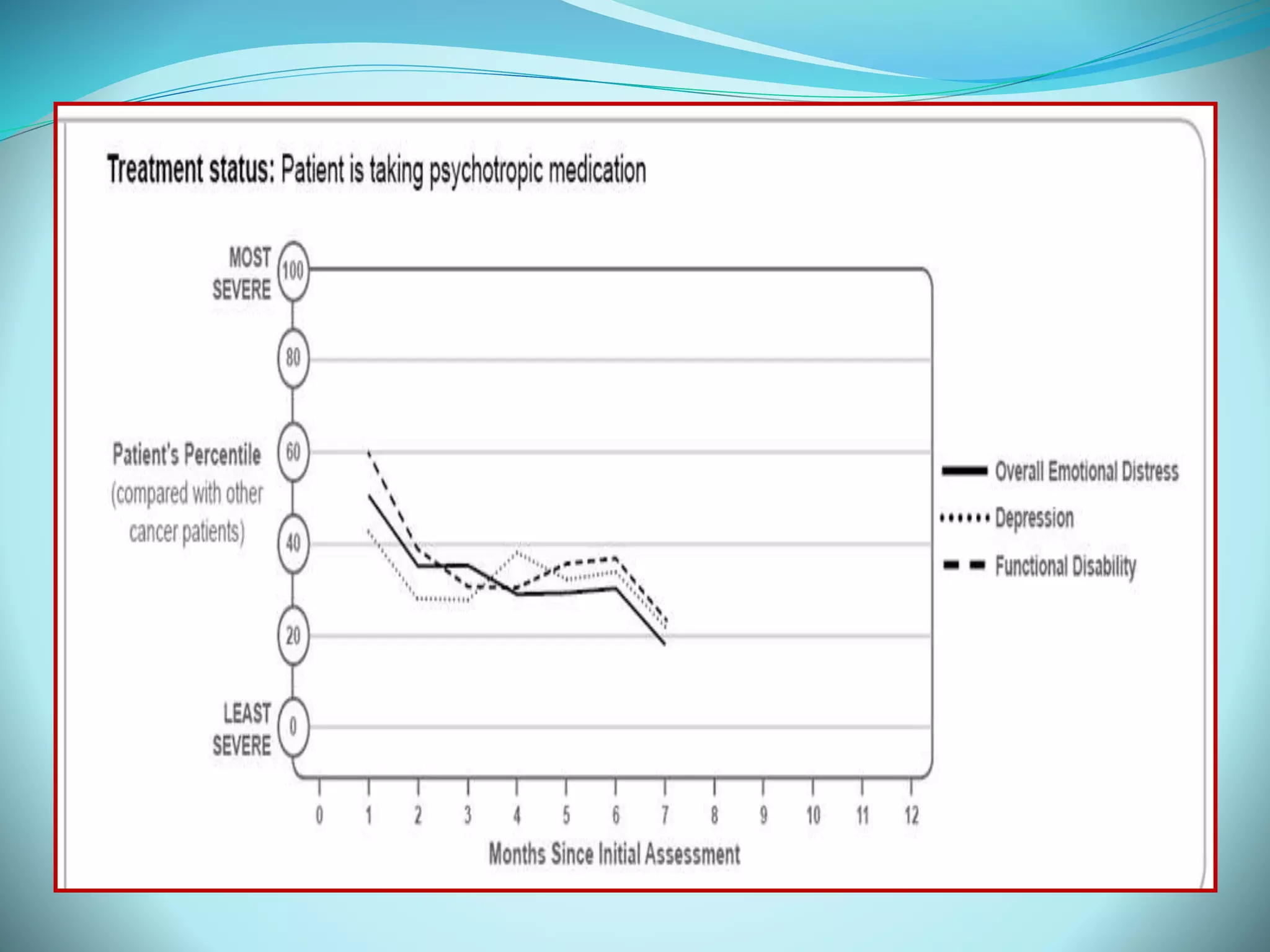
The document discusses the development and validation of the Polaris Oncology Distress Management System, which aims to address psychosocial needs in cancer care through automated assessments, real-time referrals, and tailored patient education. It highlights the system's compliance with new accreditation standards by the Commission on Cancer and its successful testing among over 1,000 cancer patients. The tool enables efficient documentation and monitoring of patients' psychosocial health, linking them to appropriate resources and support.