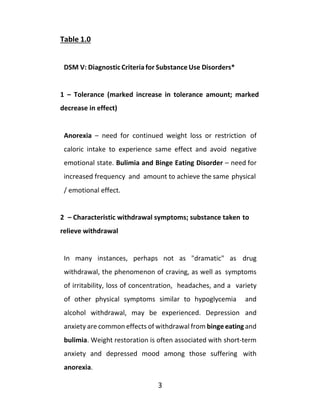
The document discusses evidence that eating disorders can be considered addictions based on criteria for substance dependency from the DSM-V and APA. It notes many similarities between the symptoms of eating disorders and the seven criteria for substance dependency/addiction. The document also discusses research showing deficits in dopamine levels and receptors in the brains of those with eating disorders and addictions, suggesting underlying biological similarities.



![The second section begins to explore the commonality of eating
disorders and attempts to debunk the belief eating disorders
represent separate and different disease entities. The common
thread existing among the various flavors of eating disorders is
reviewed and the trap of focusing on weight, appearance, and
dieting is exposed. Setting the stage for treatment thus begins with
defining the problem.
The third section begins to look at the recovery process at
Milestones. By distilling the basic elements of long-term recovery,
participants in the program learn about, and most importantly
practice, a set of skills that virtually guarantees freedom from
addictive relationships with their eating disorder. In doing so, “one
day at a time” the physical, emotional, and spiritual symptoms
inherent with an addiction begin to change course and recovery
follows.
The fourth section focuses on maintaining your recovery and how
S.E.R.F (Spirituality, Exercise, Rest and Food Plan) can assistyou.
The fifth section of this book is devoted to continuing care and the
role of support groups such as OA [Overeaters Anonymous],
Anorexics and Bulimics Anonymous [ABA], Alcoholics Anonymous
[AA], Narcotics Anonymous [NA], etc. can help you maintain your
recovery.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-5-320.jpg)







![2
“Addiction is a primary, chronic disease of brain reward,
motivation, memory and related circuitry. Dysfunction in these
circuits leads to characteristic biological, psychological, social and
spiritual manifestations. This is reflected in the individual pursuing
reward and/or relief by substance use and other behaviors. The
addiction is characterized by impairment in behavioral control,
craving, inability to consistently abstain, and diminished
recognition of significant problems with one’s behaviors and
interpersonal relationships. Like other chronic diseases, addiction
involves cycles of relapse and remission. Without treatment or
engagement in recovery activities, addiction is progressive and can
result in disability or premature death.” *American Society of
Addiction Medicine, 2012
To see if “the shoe fits”, you might take the quote above and simply
insert the phrase eating disorders in lieu of the word addiction.
Likewise, the words restricting, purging, binge eating, and so forth
could be inserted. In my professional experience, the shoe fits
quite well. It may be time to look at an eating disorder with respect
to its’ real nature rather than surface appearances. The
implications for treatment and long-term recovery areprofound.
Let’s take a moment and review the seven criteria the APA lists as
symptomatic of dependency [aka addiction]. I’ve added a few
comments for each criterion relating it to an eating disorder.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-14-320.jpg)

![5
6– Social, occupational or recreational activities given up or
reduced
Common to all eating disorders – social isolation, as well
as, diminished activities that interfere with eating disordered
patterns.
7 – Use continues despite knowledge of adverse
consequences (e.g., failure to fulfill role obligations, uses when
potentiallyphysicallyhazardous)
Common to all eating disorders – continued eating
disordered behaviors, despite physical, emotional, social, o r
financial consequences.
*DSM IV R- American Psychiatric Association/American Society of
AddictionMedicine
*Meeting a minimum of three criteria is sufficient for a diagnosis
of substance dependency [DSM IV-R]. DSM V-now defines a
substance use disorder with three subtypes: mild, moderate, or
severe. See: DSM V SUBSTANCE USECRITERIA
In recent years the addiction model, at least as it applies to bulimia,
binge eating, and anorexia has been the subject of an expansive](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-17-320.jpg)
![6
body of research. A terrific summary of this appears in the newly
published text “Food and Addiction” edited by Kelly Brownell and
Mark Gold, Oxford University Press, 2012. The concentration of
this effort has ranged from an exploration of the nature of certain
properties of [mostly refined] foods to the neurobiology and
physiology of [eating disorders] addiction. There appears to be an
interaction between the nature of the substance [addicting or non-
addicting] and the nature of the person [addict or non-addict].
Hence, it is difficult to pin the blame only on the substance without
consideration of the person. For example, morphine is quite
addictive but not all patients receiving this drug to control pain
become “addicts.” Still others, who have a history of addiction, are
more vulnerable to becoming dependent on the drug. We know
today sugar and its’ many derivatives is addicting as a substance.
However, addiction to sugar is both dose and length of exposure
dependent, as well as, being influenced by the person consuming
it. This is to say it takes “two to tango” - with the substance needing
to interact with a predisposed and willingsubject.
The most compelling evidence to date seems to have come to light
with the brain mapping capabilities of modern radiographic
imaging (PET Scan/brain imaging). Sparing the reader the technical
side of this, researchers have been able to locate and display areas
of the brain reacting to substances and stimuli in ways that
differentiate the addict from the non-addict. Furthermore, we now](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-18-320.jpg)
![7
better understand the “reward system” in the brain. We can clearly
see differences between dependent and non-dependent subjects.
Dopamine has been shown to be a primary “feel good” chemical in
the brain. Researchers have uncovered a stunning similarity
between chronic cocaine and stimulant abusers, and compulsive
eaters and bulimics – namely all have shown deficits in dopamine
concentrations and dopamine receptors on their PET scans. The
control subjects [non-addicts] did not display the same deficits. In
yet another study, the two groups were exposed to just pictures of
cocaine or, for overeaters, highly palatable desserts. The visual
cues alone caused a marked increase in dopamine activity among
the cocaine and ED subjects, but not so with their non-addict
peers. So, both an external cue [visual], as well as, the actual
consumption of the substance can elicit changes in brain
chemistry. This is what behaviorists call classical conditioning.
I’ve included an article I wrote summarizing the chemistry involved
with many eating disorders. The focus of the article looks at the
role of one of the basic neurotransmitters we spoke about –
dopamine. As mentioned, dopamine has been studied with respect
to its role in addiction. The progression from use, to abuse, to
dependency likely involves the interplay of amount, duration, and
individual predisposition – whether we speak of a drug or an eating
disorder.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-19-320.jpg)
![8
Dopamine- the “Feel Good Brain Chemical”*
In an article on the role of dopamine and dopamine receptors from
a March 2010 edition of "Neuroscience" - a well-known and
respected professional journal, the researchers found a significant
difference between laboratory animals that were "over-fed" and
exposed to unlimited amounts of sugar laden and highly processed
[junk] foods versus controls fed regular rat chow. Indeed, the junk
food rats developed an "addiction-like reward deficit" with
dopamine concentrations. The virtual destruction of D2dopamine
receptors in the brain accounts for this.
Translation - over time, when overeating highly "palatable" foods
(e.g. sugar, high fat) they [rats] developed deficits in their ability to
properly assimilate the neurotransmitter dopamine. Deficits in
dopamine are seen with cocaine addicts when they are "crashing"
and withdrawing from cocaine - they become depressed and their
appetite becomes almost insatiable. Likewise, the deficit in
dopamine for binge eaters and bulimics tends to increase over
time with the result being a biological (addictive) propensity to
repeat episodes of disordered eating with greater frequency. Of
course we’ve come to know this phenomenon as tolerance. For the
bulimic, the misguided attempt to deal with this is purging or
alternating between periods of binge eating and restricting, for the
compulsive overeater, controlling this addictive cycle gives way to](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-20-320.jpg)
![9
another "diet". Whether this mechanism plays a role with forms of
anorexia is still a subject for speculation. I suspect the addictive
process with restricting is similar.
Much like the cocaine user who becomes an abuser and then an
addict, neurotransmitters (dopamine receptors) are eventually
destroyed. The only relief is...more cocaine for the fewer receptors
available. The phenomenon of tolerance takes hold and theaddict
needs more of the substance to achieve the desired effect until no
matter how much substance is available it no longer works as it did
in the beginning stages. In fact, in most end stage addictions the
best one can hope for is to postpone withdrawal symptoms.
Addiction thus becomes a full-time career.
The "food addict" may begin abusing food and develops a similar
"tolerance" to refined carbohydrates (sugar, flour) or greater
volumes of food and, likewise, alters the brain's (reward) structure
(dopamine receptors) and the physical addiction to overeating
takes hold. A similar mechanism exists with purging, as applied to
endorphin metabolism. With anorexia the starvation process
creates a sort of tolerance as the body fights to survive and the
anorexic must restrict more and more to maintain the sameeffect
[e.g. avoid weight gain and control despair and anxiety]. Thereare
a few studies to suggest the stress hormone cortisol plays a rolein
this process much like the neurotransmitters in the brain.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-21-320.jpg)
![11
As with cocaine addicts, it's likely that over any extended period of
time, the mechanisms responsible for manufacturing and making
available dopamine at normal levels will re-emerge... provided the
"addict" adheres to a prescribed course of treatment (e.g. abstains
from the offending substance - cocaine or, for the food addict, the
combination of high-glycemic foods and over feeding [exorbitant
volume]. Likewise, proper nutrition and restoration of a
reasonable BMI would likely have a similar effect for the restricting
forms of eating disorders.
The first step in recovery is recognizing the importance of
abstaining from the offending substance[s] and behavior[s]. Those
with an eating disorder may need to consider a food plan that does
not evoke a physical craving. The current body of research suggests
the more highly processed a food substance is the more likely it is
to heighten the potential for abuse and dependency. The
exponential increase with childhood obesity and early onset
diabetes is directly related to this phenomenon. The evidence has
become overwhelming.
References:
Marty Lerner, PhD .2012
http://www.selfgrowth.com/experts/marty-lerner-phd
Laboratory of Behavioral and Molecular Neuroscience, Dept. of
Molecular Therapeutics
- Published 3/2010 in Nature Neurosciences
Neuroanatomy of Addiction, George Koob, 2012 in Food and
Addiction by Brownell and Gold, Oxford Press, 2012](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-22-320.jpg)

![13
related to alterations of interceptive awareness. There may be
some disregulation of insula function. This may, in part, explain
why a recovering anorexic can draw a self-portrait of their body
image that is typically 3 times its actual size.” To quote from
someone with this experience who is now recovering, “I was down
to 80 pounds at five-foot six,” she says. “My self-portrait was so
distorted I was able to lie down inside the drawing, but that’s how
I saw myself."
A reprint from an article published in Bloomberg News serves as
an excellent summary of the evidence pertaining to the addictive
nature of highly processed [junk] foods. Written by investigative
journalists Robert Langreth and Duane Stanford, the article
explores the social, economic, and biological impact of food
addiction and provides a rather convincing indictment of the
companies profiting from these products. Here is a [reprint] of the
Bloomberg article
The Case for Commercial FoodAddiction
REPRINT- Bloomberg News, April 2011
Robert Langreth and Duane Stanford, investigativereporters
A growing body of medical research at leading universities and
government laboratories suggests that processed foods and sugary](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-25-320.jpg)













![29
Defining the Problem…
Ok, let’s take a moment and “think outside the box” and ask what
all these different “flavors” of disordered eating have in common
rather than what separates them? Is it not true most people,even
medical and mental health professionals, tend to identify and
define an eating disorder in terms of how someone looks or how
overweight or underweight they appear? After all, how can one
suffer with an eating disorder if they don’t appear eating
disordered? And, how is it possible someone can admit to having
an issue with abusing food, excessive dieting, or compulsive
exercising, and not show outward signs?
Even more striking is this perception is too often supported by
many of the treatment programs and self-help groups intendedto
help people find their way into recovery. In effect, this seems to
overshadow the fact that, recovery is about more than just
changing someone’s weight or eating behavior. For most people
with a bona fide eating disorder, body weight and body image
perception are a set of symptoms and [excuse the pun] not the
whole enchilada. Fact is, not all underweight people suffer with
anorexia and not all overweight people suffer with a binge eating
disorder. Suffice it to say there may be a difference between a
weight disorder and an eating disorder. Again, I refer the reader to](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-41-320.jpg)
![31
the APA guidelines [criteria] for dependency to delineatebetween
a weight problem and an eating disorder. (See ChapterOne)
It would seem many people who do not have first-hand experience
of an eating disorder “miss the boat” in this respect. Truth be told,
this is similar to what most people once believed about alcoholism
and drug addiction: alcoholics all wear sneakers, trench coats,and
live under bridges, while all drug addicts live on the streets and
steal money for drugs, and so on. We know differently today. The
overwhelming majority of chemically dependent people cannot be
“picked out of a crowd.” That said, I’d suggest we revisit the
stereotypes many of us have with respect to eating disorders.
This leads us to a retooling of the defining characteristics of all
eating disorders and an assumption I would present to the reader
for consideration.
Eating Disorders are best defined by the degree the relationship
with food and/or body image diminishes the quality of
someone’s life.
A helpful suggestion for newer members of 12-Step programs is to
“identify and not compare.” The reasoning behind this suggestion
is to not provoke the newcomer into a form of denial by telling
themselves something along the lines of “I’m really not as bad as”](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-42-320.jpg)

![32
another member. The effect of one person’s experiences shared
with a fellow having the same experiences is, to quote a related
program, “unparalleled.” Once the initial layer of the onion is
peeled, namely the “what makes me different than these people,”
the stage is set for identification rather than comparison. The
question then becomes, “so what do I have in common with
everyone here?” From that point forward, the focus begins to
center more on the solution – “what do I need to do to recover?”
Doing otherwise leaves someone with over analyzing the problem
and little energy left to begin work on the solution.
*OvereatersAnonymous[http://www.oa.org]
*AnorexicsandBulimicsAnonymous[http://aba12steps.org/]
Aside from meeting at least three of the criteria for dependency
we read about in the previous section, eating disorders tend to
have in common the relentless attempt to control how we feel.
Although we’ll look at this more in depth in the next section, I
would suggest that all eating disorders are motivated by an intense
desire to fix or avoid an unpleasant feeling. Although the feeling
may vary within and among persons, the end game remains the
same – control, fix, and change the feeling / discomfort du jour.
One variant on this theme comes from a summary statement made
by a very famous psychoanalyst, Carl Jung. Although I may be](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-44-320.jpg)

![34
Over time, too much avoidance and distraction have the potential
of becoming addictive, as our tolerance for discomfort becomes
less and less and our need to find relief grows stronger. Unless we
find a more appropriate and less destructive means of reacting to
“legitimate suffering” we are prone to creating a number of
compulsive and addictive behaviors.
Although I would hardly count myself in the same category as Carl
Jung, I do believe he was on to something back in his day. After all,
people do not starve themselves, make themselves sick, take
handfuls of laxatives, binge eat until they’re in pain, exercise to the
point of exhaustion, or engage in any number of painful actions
unless they are attempting to avoid or change their emotional
state. As mentioned, what we see with eating disorders is a
progression of first attempting to feel better followed by an
attempt to delay or avoid feeling bad [withdrawal] in the later
stages. I’ve seen this to be as true for someone in the midst of
anorexia as someone struggling with a binge eating disorder. The
same can be said for almost alladdictions.
Another similarity within the ED population has to do with the
incidence of coexisting mood disorders. More often than not
recurring depression, anxiety, and marked mood swings come with
the territory. In addition, more than half the people seeking
treatment have histories of abusing alcohol, drugs, and/or other](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-46-320.jpg)
![35
forms of self-abusive behaviors like cutting. Regardless of the
particular eating disorder, it’s rare to see someone with an ED
without an accompanying mood disorder, chemical dependency,
or self-abuse issue.
Table 2.1
Similarities among the EatingDisorders
- The majority of people with an ED meet the established
criteria for [addiction] dependency per the same criteria
typically reserved for substance dependencies*.
- ED behaviors are initiated in an attempt to avoid or change
uncomfortable feelings - usually negative feelings and
emotional states.
- Most eating disorders typically are associated with a mood
disorder that often pre-dates the beginning of the eating
disorder.
- Regardless of ED type, at least half the people coming to
treatment for an ED also have abused alcohol, drugs, or
relied on additional forms of self-medication.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-47-320.jpg)
![36
- Having an ED makes someone vulnerable to “switching
addictions” throughout the life cycle of their ED.
- Independent of the form of ED, control issues are a central
theme needing to be addressed – first with food and
weight, and later with other areas of daily living such as
relationships.
- With the exception of some subtypes of anorexia, most
people suffering with an eating disorder react to certain
foods [e.g. sugar derivatives, refined flours, highly
processed junk foods, etc.] differently than their non-
eating disordered peers. *see D2 receptors and eating
disorders
- Both psychological and physiological factors are inherent
among all forms of eating disorders. Physical dependency
and psychological dependency interact to create an
addictive relationship with food, body weight, and/or
dieting.
- Long-term recovery from an eating disorder requires
significantly more than a temporary change in someone’s
body mass index [BMI / weight / appearance] and eating
pattern.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-48-320.jpg)
![37
- Recovery often requires the ongoing participation in a
support group or a continuing care plan after formal
treatment ends.
- Appropriate [non-habit forming] medication[s] usually are
needed to treat co-occurring depression or a similar issue
accompanying an eating disorder. In many instances, the
mood disorder is a “stand alone” diagnosis that exists with
or without the ED.
- Most people with an eating disorder have some level of
impairment with an ability to differentiate between
hunger [physical needs] and appetite [psychologically
driven]. – internal versus external cues of hunger
- As with other addictions, remission is a more realistic
expectation with treatment outcome rather than a “cure.”
In effect, addiction is a life-long disease that can be
arrested by remaining engaged in consistent recovery
related activities. Remission can be life-long or short-term.
Co-Existing Addictions and RelatedProblems
Those of us who have been in and around the recovering
community are quite aware of the prevalence of eating disorders
within the fellowships of Alcoholics Anonymous, Narcotics](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-49-320.jpg)




![43
Cross Addiction and Co-Existing Issues
The take away from this topic is simply to recognize addictions and
compulsions are often misguided attempts to manage or control
our feelings. That being the case, it would seem likely when we
stop using one means of doing this we’re prone to “go back to the
well” and rely on another. The important thing here is to accept
the need to work on the problem [nature of the person] and not
just the symptom [the addiction]. Be patient, be cautious, and be
honest with yourself. Some of these issues can be tackled along
with your eating disorder treatment and some will be taken on
later in the course of your recovery. Which one and when will
depend on how they threaten your eating disorder recovery and
whether you can “buy time” to work on them at a later date.
Body Image and Body Dysmorphic Disorder
I’ve always been fascinated by the “disconnect” between how we
experience our speaking voice and how it sounds when we listen
to it from a recorded device. Likewise, there’s the tendency to view
different photographs of ourselves and wonder how we could look
so different in each one, yet almost everyone else hardly notices
any change. How can we see the same picture so differently from
others? Is it possible our perception is influenced by factors we’re
not totally aware of? To be clear, this phenomenon of perceiving
and experiencing ourselves differently from the “outside world” is](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-55-320.jpg)


![46
of ourselves. The “smoke and mirrors” effect of an eatingdisorder
then goes something like this: “I look in the mirror and I see myself
as and that’s what really makes me feel depressed. If I were
able to change the way I look then I wouldn’t be so depressed.”
Hence the anti-depression fix becomes changing the body or
numbing the pain with further restricting or binge eating, etc. The
angst of how we experience our body is believed to be the problem
and the solution becomes changing the body at any cost – evento
the point of engaging in life threatening behaviors.
I’m not proposing the solution to a body image issue is simply
“buying into” this theory or finding the right “medication.” What I
would suggest is at a minimum conceding your “perception” is a
confused one and giving consideration to putting your energyinto
a recovery process. That process would give equal time to
following a treatment plan that includes a healthy food plan,
abstaining from your eating disorder behavior[s], with professional
help if necessary, and also finding a way to appropriately manage
your depression. Last, but not least, I would be remiss not to
mention that more than half of the people we see at Milestones
also have relied upon alcohol, drugs, or other compulsions in
addition to their ED in a misguided attempt to “control” their
depression and perceptions.
In sum, body image disturbances are a prominent feature of most
eating disorders. Whether they are a symptom of an underlying](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-58-320.jpg)
![47
issue with a mood disorder such as depression or generalized
anxiety disorders, a manifestation of past trauma, or any number
of factors often associated with eating disorders may not be
important. What matters is the need to acknowledge body image
disturbance as a symptom of the disease – more so for some, and
less so for others. Another point to consider is resolving the
depression or underlying mood disorder does not guarantee the
resolution of a distorted or negative body image. That said feelings,
thoughts, and perceptions about our body become less
troublesome over time if following a recovery program. By
incorporating the principles of a 12-Step program and some ofthe
principles discussed, we can learn to live with our imperfections.
The frequency and intensity of negative experiences with our body
will diminish. Self-focus and a renewed interest in other people
and things beside ourselves will usually follow.
Internal and External Cues: What also makes usdifferent?
My experience has been eating disorders almost uniformly involve
a broken thermostat-like mechanism that governs internal cues
[symptoms] of hunger and fullness. In other words, unlike our
“normal eating” contemporaries, we are often confused when to
eat, what to eat, how much to eat, and/ or when to stop eating.
Whether suffering with anorexia, bulimia, or compulsive
overeating, there is a tendency to be more governed by external
stimuli - such as the sight of food, smells, time of day, stressful](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-59-320.jpg)




![52
to as a cucumber becoming a pickle never to return to being a
cucumber again. Being a pickle, however, does have its
advantages. With acceptance of our reality, the adoption of a
reasonable food plan becomes a preferred place to be ratherthan
a prison sentence. *Clean eating, along with the other components
accompanying a recovery lifestyle become a matter of preference
and not something we do because “we have to.” You’ll find the
same experiences among people enjoying long-term recovery
from alcohol, drugs, and other dependencies - namely their
“recovery” has become a blessing and not a curse. I’d further the
analogy to someone with any chronic disease. If we we’re
discussing diabetes treatment then eating within the bounds of a
healthy whole-food plan, moderate exercise, managing stress, and
developing a personal sense of spirituality would be the exact
prescribed program called for. If you think about it, this formula
would serve anyone with a chronic disease and go a long way to
restoring someone’s health and quality of living.
[*]It’s important to remind the reader our reference to “abstinent
food plans” and “clean eating” are about healthy and adequate
nutrition and not in the service of further restrictingcalories.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-64-320.jpg)


![55
no cigar. Eventually you might get it to close with one or two eggs
left. Not much recovery left here. Maybe your SERF is reduced
to EF.
And now…. Take an identical size bowl that’s empty and place it
next to the original one. Now take all four [SERF] eggs and place
them in the empty bowl FIRST. Now pour the same rice from the
original bowl over the eggs on the bottom. And, finally, place the
lid on the bowl. Guess what – it fits.
Believe it or not, this is something we actually do as a
demonstration from time to time at Milestones. In reality, we’ll
find ourselves with more than enough time to take care of what
needs doing when we put our recovery first and allow the rest of
our daily stuff to fall into place. Being consistent with the SERF
basics is one of the paradoxes of recovery – namely putting
ourselves first-positions us to better take care of everything else.
As has been mentioned repeatedly throughout this guide Doing is
Believing.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-67-320.jpg)

![57
The Roadmap
When all else fails, follow the directions” – anonymous
Ok, now we’ve come to the instructions. You know, the written
materials [aka instructions] most people either discard or only
glance at while putting together whatever it is they’re trying to put
together. If you’re like me, you usually end up with a bunch of parts
left over and something that doesn’t quite look like the picture on
the box. This may be a time to do it differently. A word of caution
- it’s not unheard of for people with, shall we say, control issues,
to be slightly defiant and a tad bit stubborn [a little sarcasmhere].
If this doesn’t apply to you then I would suggest you may be inthe
wrong place or, more likely, are having one hellacious issue with
denial. Fact is, most people who suffer with an eating disorder,
have more issues with control and trust [what a surprise] than their
non-addict peers. These two issues are a central theme of what
needs to be addressed in the recovery process. We’ll talk about
control and trust in a few pages.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-69-320.jpg)




![63
sustainable lifestyle. Many refer to this as a
recovery lifestyle. The program follows a
"blended" approach to treatment - addressing
both the addictive and emotional aspects of an
eating disorder. Residents attend a fullschedule
of group and individual activities during the day,
as well as, participate in various support groups
during evenings and weekends. Grocery
shopping, meal preparation, and "real world"
experiences are an integral part of the
program.” [*]](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-75-320.jpg)



![68
At first glance these concepts may seem simple enough. However,
there is more to this stuff than meets the eye. There seems to be
an implied assumption in the world of mental health treatment
that goes something like this: if we can change how someone feels,
or if we can change what thoughts they have, then we can get
someone to change what they’re doing. I suspect most of us hold
onto the belief that goes something like this - if a therapist or
someone I looked to for help could fix how I feel, then maybe I
would be able to _. You fill in the blank. Try this one on for
size: “If or when you can help me feel better about my body I will
buy shorts and exercise.” “When I don’t feel so big I’ll let myself
eat.” "When I’m not so nervous, I’ll speak in front of the class and
be able to do the presentation.” “When I get [aka feel] motivated,
I’ll study.” No doubt we can make an endless list of “when I feel, I
will.” Experience has shown repeatedly when we put a “state of
mind” as a condition for doing something we’re likely to be stuck
in the problem. Conversely, when we develop the discipline of
doing what needs doing despite the feelings or intrusive thoughts
we are moving toward the solution. Let’s take a few minutes and
look at the basic principles of this philosophy and explore it. I’ve
taken the liberty of paraphrasing some of the CL principles David
Reynolds talks about in his text. They are:](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-80-320.jpg)
![69
- Feelings are not directly controllable by self will
- Feelings need to be recognized and accepted “as is”
- Every feeling, no matter how unpleasant, has a
purpose
- Feelings fade over time, unless re-stimulated
- Feelings [and thoughts] can be indirectly
influenced by behavior
- We are responsible for what we do no matterhow
we feel
If you really consider these, they tend to appeal to our common
sense and really don’t require a degree in rocket science. However,
taking a more detailed view and truly contemplating these you’ll
notice a much more profound meaning. What is being proposed
are a set of what could be called, universal truths about the human
mind and how it operates. It suggests trying to control our feelings
by directing energy into simply “willing” ourselves to feel
something is a wasted exercise. Try sitting down in a chair when
you’re feeling sad and “will” yourself to feel happy for any
extended period of time. Try willing yourself to fall in love with
someone you’re not in love with. Likewise, controlling your
thoughts by imposing self-will is quite limited as well. Ever tell](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-81-320.jpg)
![71
yourself not to think about something? I usually end up obsessing
about something the more I try or am told not think about it. The
“magic sauce” in all this is that our thoughts and emotions can be
indirectly influenced by what we do. In other words, what we do
has the greatest [probable] impact on what we think and feel over
time. The cart is placed before the horse when we get it backwards
by insisting we fix our feelings first. Believing our feelings and
thoughts must be changed before we’re able to change our
behavior can be a very costly mistake.
Once again, eating disorders and addictions are about fixing
feelings. Now we can add another idea, this time regarding the
solution – “recovery is about transcending our need to fix how we
feel and doing the next right thing no matter what we’re feeling.”
This challenges the belief that controlling our feelings and thoughts
is the primary goal of psychotherapy. Instead we’re proposing the
reverse - controlling our actions and letting the feelings and
thoughts take care of themselves. “Doing is believing” as I like to
say.
Feelings and thoughts, as we’re reminded, are never constant.
Much like weather patterns, our emotions and thoughts are always
changing. They come and go. In this sense, nothing stays the same.
Trying to exert control over these is like trying to control the
weather – not possible. Behavior, with very few exceptions is](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-82-320.jpg)


![73
The dateline is eighth grade at Lawrence Junior High School
somewhere in New York. I am about 14 years old and suffer with
what was, at the time, referred to as juvenile onset obesity. In
other words I was a compulsive eater who was twice the size of
what would be considered “normal” for a 14 year old. So nowinto
the classroom enters Paula Goldberg, a very “hot” looking 14 year
old dressed in a mini skirt and knee high boots. No doubt you get
the picture. Kind of like the scene from the “Go Daddy.Com”
commercial with the supermodel and computer geek in a lip lock.
Fast forward the movie and I began a “diet” of raisins, cottage
cheese, and diet soda for the next several months until I became
this rather good looking, “svelte,” high school freshman. Now,
eventually, I ask Paula out to the junior, then senior prom.
Throughout high school we were, as they say, an item.
Comes time for high school graduation and off to college. Now
we’re both about to go to different colleges. I figure it’s time for
me to “sow some wild seeds” and not limit myself to Paula. I figure
it’s time to break up with her. Here’s where it gets a little
interesting. I invite her to meet me at the Town Diner [remember
Harry, this is the same place].
So we sit down at the table and Paula says she wants to tell me
something. I tell her “I have something to tell you too Paula, [big
mistake here] but instead I tell her “you go first Paula.” Paula
proceeds to tell me “Marty, you know I care about you, but I think](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-85-320.jpg)






![81
need to do recovery.” By doing so, your perceptions and thoughts
are likely to be reshaped and indirectly influenced by your actions.
You can again accuse me of butchering another famous quote by
restating it as follows: “I think I am, therefore I am” might be better
stated as “I do, therefore I am” – from that perspective, we tend
to be defined by what we do and not so much by what we say or
feel. Another cliché popular within recovery circles is “we are
judged not so much by our intentions as by our actions.” I know
very few people who get in trouble for what they think or feel, but
plenty who get into issues for what they do. Conversely, proper
action can produce amazingly good results in spite of feeling and
thinking negatively. More than likely the negativity will change
over time if the behavior is positive.
Being realistic about this “just do it” discipline is important. Doing
what needs doing does not always guarantee feeling good or
getting rewarded in accord with your expectations. Here’s a case
in point. I remember trying to put these concepts into practice
some time ago and came home one day to find a bunch of dishes
in the sink that my wife had yet to clean. Ok, I’m [feeling] resentful
that I’ve worked all day and here are dirty dishes that need to be
washed and [I think] my wife is supposed to wash the dishes.Alas,
I am now Mr. CL and will put on my CL outfit and wash the dishes
despite feeling crappy and resentful. Now that I’ve done the dishes
I am expecting my wife to be so overcome with gratitude that she’ll](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-92-320.jpg)






![88
rather following a prescribed program (as noted above) and letting
go of the outcome – namely not making changes in response to
feelings, fears, or temporary changes in our bodies. Allowing
someone other than us, at least in the beginning, direct our food
and exercise plans is a far more objective and ultimately successful
means of finding a solution to the mental tyranny of trying to do it
alone. To be sure, it takes a quantum leap of faith and courage to
“turn over” control to someone other than yourself. In the end,
sponsorship in an appropriate support group such as OA or ABA,
making good use of a trusted and experienced professional, and
cultivating a belief in your own understanding of a higher power
will put you on the path to reclaiming your life”.
Marty Lerner, Ph.D.
It’s All About the Food…Isn’t it?
A food plan is not meant to be a “diet” in the traditional sense of
the word. It is better viewed as akin to comfortable clothing rather
than a straightjacket. It may change and be adjusted over time and
is not a “quick fix” or the be all and end all to treating an eating
disorder. However, it is an integral piece of the recoverypuzzle.
Although the term abstinence refers to the cessation of eating
disordered behaviors, whether binge eating, restricting, purging,
and so on, it also can refer to the specific boundaries regarding
properties of foods [types and amounts] within the plan. In](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-100-320.jpg)



![92
“SERF” and not with manipulating the body to reflect a certain
number or conform to the body image du jour. The “trust” and
“control” issues we spoke about before have to do with trusting
your body’s response to a healthy food and exercise plan and
letting go of trying to control your body’s set point at any cost.
The measuring aspect of recovery as it relates to the food plan is
to weigh and measure our food and not our bodies. Doing so
avoids the tendency to over or under do what’s called for on our
food plan and serves as a teaching tool. It is not intended to
aggravate our compulsive nature, but rather to focus on following
a part of our recovery plan. Whether one continues to do so after
a few weeks or months of recovery becomes an individual choice.
Perhaps the same can be said for being weighed periodically by
yourself or someone else. If the benefits [excuse the pun]
outweigh the negative effects, fine. For most people, relying on
other measures of what’s happening with our bodies such as how
our clothes are fitting, etc. are enough.
Measuring Recovery – How am I Doing?
This is a really short topic. I would encourage anyone with an
eating disorder, or any addiction for that matter, to measure
progress in terms of how one is doing rather than how one maybe
feeling at a given time. Quite frequently, we may be feeling bad](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-104-320.jpg)


![95
S.E.R.F. Lessons
Let’s see how many metaphors we can come up with for the SERF
stuff. “Stay close on your SERF board or you might drown.” Ok, ok,
how about – “The key to SERF-ing is all about balance” – I likethat
one. I’m done. Thanks for indulging me.
Spirituality – Give me an “S”
A quick disclaimer, I am no guru or authority on the subject
of spirituality. In the context of eating disorder recovery Iwould
suggest spirituality is, however, an integral part of ongoing
recovery. Defining spirituality is, at best, ambiguous. That may
be a good thing since there are no rules or religious dogma
attached to its practice. It affords anyone and everyone an
opportunity to participate. So let me attempt to bring together
two concepts that permeate the 12-step addiction recovery
literature – spirituality and powerlessness.
First, allow me to quote from Elisa Goldberg’s workbook used as
a text for her course on Spirituality in Behavioral Health Care
Settings [Drexel University -October, 2013].
“Spirituality is an essential element of human experience. It
represents the part of us that searches for meaning, seeks out](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-107-320.jpg)



![99
Just as an aside, our bodies respond to excessive exercise and
activity [burning too much energy] with fighting for survival. It does
so by conserving energy. Thus, too much exercise and your body’s
metabolism will slow down in an effort to fend off starvation and
tissue loss. In other words, too much exercise and too little food
begins to demand more exercise and less and less food to maintain
continued weight loss or prevent weight gain. Anyone remember
what symptom of addiction this refers to? That’s right – it’s
TOLERANCE. Developing tolerance requires more of the same
behaviors or substances to achieve the same effect. I guess we
could say again this is about “getting caught in your own mouse
trap.” Likewise, the loss of a regular menses signals the body is not
able to withstand the rigors of child bearing while in survival mode
and protects itself by slowing down energy expenditure,
decreasing sex drive, and reverting the body back to an almost pre-
adolescent state.
With the “too little exercise” end of the spectrum, we are caught
up in the spiral of inertia. With an inadequate amount of activity
the body responds in ways that make it ever more difficult to dig
ourselves out of the hole we’ve dug. Our metabolism slows and
our energy levels decrease. We can find ourselves developing
metabolic diseases such as adult onset diabetes [Type II Diabetes]
with increasing insulin resistance. Our overall muscle mass](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-111-320.jpg)
![101
decreases and we begin to associate feeling exhausted with
“thinking” we need to feed ourselves.
Moderate exercise is difficult to figure out objectively when in the
midst of an eating disorder. Like hunger perception and body
image, it can be confusing at best. With the amounts of food, we
tend to overestimate and under estimate what’s needed for our
recovery. It’s best to have someone with experience suggest a
reasonable exercise / activity plan along with a food plan in the
beginning. Individual needs will vary in accord with ones’ level of
fitness, their body mass, medical history, and so on. Suffice it to
say, moderate exercise should consider the following factors – for
example, frequency [3-5X weekly], duration [20-60 minutes],
intensity [60-80% of MHR]* may be guidelines.
*Aerobic intensity is usually measured by a formula that considers
someone’s age, max heart rate, etc. For our purposes, intensity can
be equated with being able to carry on a conversation while
exercising without losing your breath.
Rest – The Balance between Work and Play –
Give me an “R”
Ok, for some of us it may be “all work and no play” and of course
for others, "all play and no work.” The proper balance between
work and play is an essential piece of the recovery puzzle. I suspect](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-112-320.jpg)

![102
interpret mental stress as physical stress and think physical
inactivity is in order. Indeed, what needs doing in this instance is
rest that involves activity and movement [aka exercise]. Physical
activity serves to balance emotional stimulation and intellectual
activity balances physical exertion. Physical work necessitates
physical rest while intellectual pursuits require physical activity to
restore balance. All this may sound confusing, but will make sense
after you experience it for a period of time. Whether a person
needs rest by intellectual challenges, physical activity, or play will
vary in accord with their circumstance and daily routines.
Last, but certainly not least, is sleep. Providing yourself with
adequate time to allow for 7-8 hours of sleep nightly is sound
advice. However, it should be mentioned that almost everyone
new in recovery has some difficulty with sleep – usually not able to
fall asleep and/or stay asleep. Sleep is one of the few behaviors we
have limited control over. Over time and with continued recovery
the sleep cycle rights itself and sleep follows a healthy and
predictable rhythm. During the initial part of your recovery you
may benefit from a non-addictive medication. Short of that, I
would suggest providing yourself with ample time to rest and, even
if not sleeping, begin the habit of being consistent with a time for
sleeping. If you are having a problem with sleeping at night, know
this will pass over time. Be careful not to nap or sleep during the](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-114-320.jpg)
![103
daytime while your body is making adjustments to a sleep cycle in
sync with recovery.
Food Plans: Food for Thought – Give me an “F”
Rather than enter the “great food debate” and subject you to more
repetition of what has already been discussed, this section is
relatively short and [there’s that food pun again] sweet. The basics
[cooking pun now] boil down to eliminating sugar, flour, and highly
processed, high-glycemic foods, and controlling the volume of
food on the plan. There is also the suggestion of weighing and
measuring portions to insure accurate portions given the notorious
tendency among us to “distort” amounts.
I want to repeat once again and be perfectly clear the food plan is
not a diet, but a set of boundaries around eating. It is intended to
become a comfortable experience over time and not to function as
a set of handcuffs. The food plan is simply healthy eating,
eliminating junk foods, and insurance against either overeating or
under eating. It is subject to modification and adjustment under
the direction of someone other than you. It has an ability to be
flexible, but not at the expense of certain established boundaries.
Think of it as medication – something you neither prescribe nor
change without talking it over with the person responsible for
prescribing it in the first place.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-115-320.jpg)








![112
change others. However, we do have the ability to change
ourselves. This brings us to an important point*.
The point is to not insist on finding someone who makes the grade
or trying to force someone into becoming our version of these
attributes. The real challenge is becoming the4As.
Relationships in Recovery – “Rules of the Road”
- Water seeks its' own level when it comes to relationships. In
other words, “birds of a feather tend to flock together.” Stick with
the winners in recovery.
- Relationships do not remain the same when one or both people
in a relationship begin recovery. There is a shift in the balance of
power.
- Often acts of [responsible] independence can be perceived as
acts of betrayal when new recovery behaviors begin to emerge.
- As recovery progresses, the tendency is to trade in approval for
respect from others – aka people pleasing decreases and
assertiveness begins to replace it.
- Priorities start to shift in recovery. The need to control others
starts to diminish over time.
- The experience of walking into a room full of people and
wondering “who is going to like me” starts changing to “who do I](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-124-320.jpg)

![114
people. Perhaps something to give a little thought to - but then
take action with. The 4 A checklist can give you a general idea of
just how you’re doing "and what still needs doing.”
Compliance vs Acceptance and Surrender
A frequently overlooked phenomenon within the recovering
community, aka 12-step oriented fellowships, is a true
understanding of the subtle difference between being compliant
and truly accepting ones’ “addiction.” A growing number of
professionals, not to mention the recovering community at large,
have long understood addiction is a disease with a common set of
symptoms and characteristics. In most instances these symptoms
are both psychological and physical in nature. Whether we’re
speaking of alcohol, drugs, compulsive gambling, or the different
manifestations of disordered eating [inclusive of compulsive
eating, binge eating disorder, bulimia, or anorexia] they all sharea
similar sort of “DNA.” I would refer the reader back to the
professionals charged with defining the symptoms of an addiction
outlined earlier in this book in Chapter 1. Formulated by the
American Psychiatric Association’s Task Force on Addiction, the
consensus stands today as the “Gold Standard” for diagnosing
addiction. In effect, this is one way of restating the difference
between a bad habit and an authentic disease entity.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-126-320.jpg)
![115
Should we look beyond the substance, or for that matter most
compulsive behavior[s], we begin to see what separates those who
enjoy long-term recovery from those who tend to repeatedly
relapse. In other words, exploring the nature of the person and not
simply the nature of the substance or behavior. What follows
comes in large measure from the original works of Harry Tiebout,
M.D., and William Silkworth, M.D. Both men were pioneers in the
field who treated countless numbers of alcoholics and addicts.
Each understood the physical and psychological aspects of
addiction and, in their own way, shed light on what makes
someone suffering with an addiction different from their non-
afflicted peers.
Compliance, Acceptance, Surrender - A Process, Not an Event
Let me begin by clarifying these concepts and elaborating upon the
practical implications of each of these states of mind. Let’s begin
with the notion of compliance. To paraphrase Dr. Tiebout,
compliance refers to an individual “agreeing, going along with, but
in no way implies enthusiastic, wholehearted approval”. Usually
there is a willingness not to argue or resist and although
cooperation exists, it comes with some reservations. In other
words, one is not entirely happy about agreeing or following “the
party line.” The willingness to, let’s say abstain from certain foods,
drink, or substances is somewhat shaky. Suffice it to say it doesn’t](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-127-320.jpg)
![116
take much to shift from compliance to relapse. Although the good
doctor speculates this is an “unconscious” phenomenon, I would
disagree. Most people in early recovery have some very conscious
reservations about their “lack of power” [aka lack of control] and
insist on stepping back into the ring after a brief period of
remission. Perhaps we can say compliance is a close cousin to
denial.
Understanding the specific dynamics of acceptance is tantamount
to understanding what separates those with long term recovery
from those who experience only brief periods of recovery.
Continuing with Tiebout’s observations:
“Acceptance appears to be a state of mind in which the individual
accepts rather than rejects or resists: he is able to take things in, to
go along with, to cooperate, to be receptive. He/She is not
argumentative, quarrelsome, irritable or contentious. For the time
being, at any rate, the hostile, negative, aggressive elements are in
abeyance, and we have a much more pleasant human being to deal
with. Acceptance, as a state of mind, has many highly admirable
qualities, as well as, useful ones. Some measure of it is greatly to
be desired. Its’ attainment as an inner state of mind is never easy.”
– Harry M Tiebout, M.D.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-128-320.jpg)
![117
In my experience the transition from compliance to acceptance is
a process rather than an event. As such the period of time from
which a person moves from a compliant stance to an acceptance
state of mind varies greatly. However, I would add to Tiebout’s
thesis, getting from point A to point B is quite similar to what we’ve
come to understand as the stages we all go through upon suffering
a loss. [On Death and Dying: E. Kubler-Ross, 1969]. Letting go of
our primary “reward” or “feel good” thing is no easy task. To be
sure, it is a great loss if you suffer from the disease of addiction.
The experience of transitioning to acceptance, and to that of total
surrender, will encompass the following stages:
DENIAL
ANGER
BARGAINING
DEPRESSION
ACCEPTANCE
As with other losses, one can expect to negotiate these in a
sometimes back and forth pattern, vacillating between stages until
arriving at the final stage of acceptance. It is coming to rest at the
acceptance level that one can understand and experience the act
of surrender. It is here one can sense a lifting of the obsession, no
longer needing to struggle with abstinence, but rather finding a
comfort and rhythm to recovery. Ambivalence about recovery](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-129-320.jpg)
![118
dissolves and intervals of serenity and acceptance of “life on life’s
terms” begin to increase.
Over the years Tiebout believed this “conversion experience” is
exemplified by:
• The switch from negative to positive behavior by the
act of surrender
• The cessation of defiance and grandiosity: attaining a sense
of humility
• Surrender being synonymous with a marked change
in behavior[s].
• Surrender, when maintained, exerts a positive influence on all
spheres of ones’ life: physical, emotional, and spiritual.
In effect, getting to this stage in recovery can be viewed as the
precise moment when the tendency toward defiance and ego
driven self-control cease to function effectively. With this, the
individual is totally open to accepting reality. Honesty, open-
mindedness, and willingness replace the negativity and
grandiosity, often the least attractive personality traits common to
most addicts. As the good doctor reminds us, “the act of surrender
is an occasion wherein the individual no longer fights life, but
accepts it.” My suspicion is this process coincides with the
progression of spiritual growth. In effect, there is an acceptance of](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-130-320.jpg)
![119
humility and a healthy balance between appropriate self-reliance
and reliance on something other than one’s self [ego].
Marty Lerner, Ph.D.
The Transition Home
The most important piece of the treatment experience is the ability
to transfer your experiences to the real world, namely continuing
in recovery after returning home. No one does this perfectly. The
whole idea of recovery is not for it to become your life, but to
enable you to get a life. That being said, your success will greatly
depend on having practiced daily living skills during your time in
treatment. The actual experiences of doing the grocery shopping
and food preparation, attending OA, ABA, and other relevant
groups, following an exercise plan, finding a balance with work,
rest and play, and all the other behaviors associated with
maintaining an eating disorder free life, will enhance your chances
for continued recovery at home. To the degree your last day in a
treatment program is a close fit to your next day home, is the
extent to which you have benefited from your hard work. Once
more, intellectual knowledge of recovery has little to do with the
understanding coming from the doing part.
Continuing your recovery still involves a level of commitment after
you leave the treatment setting. Rather than propose a long
dissertation as to what needs doing for “life after treatment,”](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-131-320.jpg)
![121
suffice it to say that long-term recovery is a function of practicing
the S.E.R.F. formula on a consistent basis, as well as, working all
the steps of the 12-Step group you choose to follow. Doing this will
virtually insulate you from relapse if done on a regular basis. Like
taking care of ones’ self with any chronic illness, it will require
some effort and discipline day to day. However, as said before, it
is intended to allow you to “get a life” and not become your life.
Just put the [SERF] eggs in the bowl before the rest of the stuff that
seems to demand “all” your time and attention.
Summary
Before moving on, let’s take a moment and reflect on what’sbeen
discussed so far. Despite being a little too close to the forest
myself, I’m hopeful by now the reader has an appreciation ofboth
the nature of the problem and the suggestions for long-term
recovery.
We defined the problem in terms of the physical, emotional
[psychological] and spiritual consequences inherent with an eating
disorder. We looked at what all eating disorders have in common
rather than looking at them as separate entities. We saw the
similarities between an eating disorder and other forms of
dependencies and addictions. Looking forward, we began to better
understand the dynamics of both the disease and treatment.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-132-320.jpg)











![132
S.M.A.R.T - An Alternative or Add-On to 12 Step
Organizations?
Reprint of a “Self Growth” article written [M. Lerner, Ph.D. 2014]
In the world of addiction treatment there are several choices one
has in the way of utilizing and attending a community based
support group. Should one look more closely at what is offered to
those with an eating disorder the choices are somewhat more
limited, but none-the-less do exist. This article takes a look at two
diverse, yet complimentary approaches, 12 Step oriented
programs and the SMART Recovery program.
A detailed description of both may be beyond the scope of this
article. However, suffice it to say both “philosophies” or “beliefs”
have inherent similarities, as well as, differences. To that end, I
hope to distinguish what each brings to the table that is unique and
what they share in common.
SMART Recovery Basics
Let’s begin with what SMART (SR) stands for, namely Self-
Management and Recovery Training. In a nutshell, SR offers a 4-
Point Program [not to be confused as “steps”] that amount to 1-
Building and Maintaining Motivation, 2- Coping with Urges, 3-
Managing Thoughts, Feelings, and Behaviors, and 4- Living a
Balanced Life. SR can serve as a stand-alone approach or](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-144-320.jpg)
![133
compliment another program such as a 12-step group or
professional treatment. SR does not necessarily adhere to the
premise that one need attend meetings as part of a lifelong
process, as there is a beginning, middle and end to treatment for
an addiction. Hence once an “addict” you are not always an addict.
Another, what I believe to be very important distinction, SR is
intended to be open to support any addiction and does not hold
separate groups for compulsive overeaters, alcoholics, drug
addicts, compulsive gamblers, and affected family members.
Virtually anyone with an addictive or compulsive behavior[s] with
a desire for abstinence from these, may benefit from attendance
and are welcomed.
Having the benefit of experiencing both a 12-Step Program for
many years and, more recently becoming a trained facilitator for a
SMART Recovery group, I would say SR represents a more updated
approach to addictive problems. Although there are no bona fide
studies to support the efficacy of one support group over another,
there is ample research to support the effectiveness of the“tools”
and techniques taught in the groups. These include motivational
interviewing techniques, cognitive behavioral approaches to
confronting urges and destructive behaviors, and developing
alternate healthy lifestyles to replace addictive and compulsive
behaviors. SR encourages participants to take an active role in the
group process, and unlike the format of a 12-Step meeting, talking](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-145-320.jpg)

![135
the other is discouraged and both programs promote a philosophy
of open mindedness and seeing what works best for anyone
seeking abstinence* from their addictive substance or behavior[s].
*Both programs support abstinence, but SMART does not require
abstinence from "everything," only those substances or activities
that are selected for abstinence by the participant.
While on the topic of similarities, it’s also important to note both
programs encourage the use of medical and relevant professionals
when appropriate, as an integral part the recovery process.
Inherent with that policy is the notion SMART Recovery and 12-
Step programs are there to serve as a support network and not a
substitute for medically necessary treatment when called for.
Indeed, one may argue there is a practical difference between a
support group and a treatment program. For a substance
dependent person medically supervised detoxification may be
indicated as a life-saving procedure. Likewise, for someone in the
grip of an eating disorder, medical stabilization and a structured
setting may be necessary to gain a foothold in the beginningstage
of the recovery journey. Yet for others, the frequently associated
mental health issues, such as depression, may require the use ofa
suitable medication, and so on. Although I could go on with a list
of other relevant common denominators, I would suggest
someone approach each with an open mind and experience both
groups a fair number of times, to be in a position to choose which,](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-147-320.jpg)
![136
if not both, offer the best opportunity for continued abstinence.
Indeed, some people will choose one program over the other while
still others will see each group as offering something unique and
worthwhile – opting to attend both on an on-going basis.
To someone reading this with no prior experience with a 12-step
program, I would suggest it is, at least for me, difficult to put an
aggregate of experiences into words to adequately describe them.
What I would say, unlike SR meetings, 12-Step groups are intended
primarily for specific addictions and are not one “fellowship” but
many. In other words, alcoholics would attend an AA meeting
[Alcoholics Anonymous], Overeaters go to OA, Anorexics and
Bulimics [ABA], Compulsive Gamblers [GA], and so forth.Although
not a religious program, there is a strong current of encouraging
someone to work toward their own version of “a power greater
than themselves” or a sense of spirituality, without defining what
that should be for the individual. In this sense, the program is not
religious and purposely leaves the concept of a higher power
strictly up to the individual. To be sure, there are members who
have succeeded in these fellowships who are agnostic or atheists,
and there are no “musts” in the program as outlined in their
literature. The [suggested] steps represent a series of actions or a
progressive formula participants are encouraged to complete over
time – with the inherent belief that doing so will not only result in
continued abstinence, but also lead to a more productive and](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-148-320.jpg)




![140
Understanding Insurance and the Cost ofTreatment
A clear and concise understanding of your insurance benefits and
what will or won’t be covered for an eating disorder [or a related
diagnosis] can be both confusing and overwhelming. As an
example, your insurance may list mental health as a covered
benefit [eating disorders fall within that category], but require you
to be “pre-certified” for a specific treatment [level of care]. In
doing so, the insurance company typically will utilize a set of
criteria to determine if the severity of your eating disorder meets
their criteria for “medical necessity”. As such, it’s possible you may
have the benefit, but are denied access to the program or level of
care you are looking for.
Typically, when someone considers coming to a residential, day
treatment, or intensive outpatient program such as ours, they
participate in a clinical assessment to determine their treatment
needs. Although most insurance benefits include mental health
benefits, including a residential program, a few do not.
However, assuming you do have benefits that include the
continuum of care [residential, partial hospital, and intensive
outpatient options], the provider or program will be better able to
estimate what will or will not be approved based on the findings of](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-153-320.jpg)
![142
your clinical interview [assessment]. Often the assessment can be
conducted via a structured phone interview.
As if the above isn’t complicated and confusing enough, there is
also the matter of what your particular insurance policy requires
as a “deductible” and what your “co-pay” would be for particular
services. Usually, these will be a function of whether you are
requesting services from a “network” or “out of network”
provider. Out of network providers [facilities and providers] usually
involve a somewhat greater “out of pocket” expense on your part.
That said, the good news is that after you reach [spend] a specified
amount of your own money, your insurance will typically cover
100% of the remaining costs provided you are “certified” for the
treatment you’re requesting.
By way of example, someone coming to a program or provider
contracted with XYZ insurance, may have a $250 deductible and no
co-pay for residential treatment for an eating disorder. In this
instance, the maximum out of pocket expense or financial
responsibility for that person is limited to $250 – assuming
the insurance company’s medical criteria for that level of care is
met. Likewise, someone who has a different plan may have no
deductible and no co-pay, and hence have no out of pocket
expense. Lastly, someone who is using an out of network benefit
will likely still be covered after their deductible is met,and, in some
instances, have a small daily co-pay during theirstay.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-154-320.jpg)
![143
Given all the above variables and possibilities, it comes down to
finding someone who can verify your benefits and be able to give
you a clear understanding of what to expect. In doing so, it is
important to realize some of the answers to your concerns can only
be estimated and predicted on past experiences with your
insurance company. This is because your insurance company will
not usually commit, in advance, to a specific length of stay at a
given setting or level of care. As such, you will want to know what
contingency plan exists should your insurance company [or your
managed care company] decide you no longer need treatment at
that level of care or program.
In effect, you may want to discuss your “worst case scenario”
before you commit to a treatment program, as well as, what the
most likely scenario will be. Unfortunately, there is typically some
element of uncertainty when dealing with insurance coverageand
treatment. Your job is to minimize this uncertainty, so you can
focus on the task of recovery. Here is where the experience and
integrity of the person reviewing your insurance is so important.
This process begins with a call to the provider or facility admissions
director. Knowing the proper questions to ask is important.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-155-320.jpg)
![144
Here are a few questions to ask…
• Are you in-network with my insurance company?
If not, will you accept my out of network benefit?
• What is my out of network benefit and deductible?
• What is my daily co-pay, if any, at your program?
• What is the likely maximum out of pocket expense at
your facility for the level of care I need per day?
[e.g. residential, day treatment, or intensive outpatient]
• What can I expect my out of pocket expense will befor
the recommended length of stay
• What is the average length of stay at your program?
• Will I receive a bill for treatment after I leave?
• Will I know prior to admission what my insurance will and
will not pay for?
• Will you let me know beforehand, if there is any denial of
authorization for treatment, that I will be responsible
for later?](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-156-320.jpg)

![146
Breakfast Pancakes, Oatmeal, CottageCheese
(2 servings)
1 ½ cups rolled oats
3 tbsp. oat bran
1/3 cups cottage cheese
3 egg whites
1 tsp. vanilla [alcohol free]
Mix in blender until smooth, cook “batter” a la pancake in pan
with Pam](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-158-320.jpg)
![147
Cold Cereal extraordinary
(1 serving)
1 oz. dry cereal [corn or rice flakes, puffs, etc.]
1 cup yogurt [sugar free]
1 cup peaches [frozen]
sugar substitute [optional]
1 tsp. vanilla [optional and non-alcohol]
Mix all ingredients and place in freezer for 5 minutes…](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-159-320.jpg)
![148
Oat Bran, Apple Walnut Porridge
(1 serving)
¼ cup oat bran
½ cup applesauce
2 oz. walnut pieces
1 cup water
1 packet artificial sweetener
ground cinnamon to taste
Bring water to a slow simmer. Add oat bran and cook[stirring]
until thickened - [about 3 minutes]](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-160-320.jpg)
![149
“The Doctor’s Opinion” Pancake
(1 serving)
½ cup quick cook [instant] oatmeal
2 eggs / or equivalent egg beaters
2 tbsp. low fat yogurt
1 tbsp. low fat sour cream [optional]
2 tbsp. sugar free maple syrup [optional]
Mix until a batter [using a blender is best], spray Teflon 6” pan
with non- calorie vegetable spray [Pam], and flip over andfinish
as a pancake.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-161-320.jpg)
![151
Oat Bran Muffins
(2 servings)
2 eggs
½ cup ricotta cheese [low fat]
1 cup oat bran
2 cups blueberries
1 tsp. agave nectar [or sugar substitutepacket]
½ tsp. baking powder
1 tsp. vanilla [alcohol free]
cooking spray
Mix all ingredients and pour into muffin tins. Bake at 350degrees
for 20 minutes.
Let cool, remove from muffin tins / pan wrap tightly in plastic
wrap and store in fridge or freezer. To reheat, microwave in a
slightly damp paper towel.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-162-320.jpg)
![150
Chicken and White Bean Salad
(2 servings)
6 oz. chicken, chopped
4 oz. cheese, feta crumbled
1 can cannellini beans, canned, drained
1 cup zucchini, diced
1 cup celery, diced
2 cups lettuce, romaine, raddichio, endive
4 tbsp. olive oil
2 tbsp. vinegar, or lemon juice
6 tbsp. orange juice
1 tsp. mustard, prepared brown
1 clove garlic salt and black pepper
Dressing: Peel the garlic clove and smash with side of a chef’s
knife. Use a fork to mash the garlic with ¼ tsp salt in a small bowl,
forming a course paste. Whisk in oil. Add the orange juice,
vinegar, Dijon Mustard and pepper to taste. Whisk until well
blended. Set aside.
Notes: The classic vinaigrette recipe is 3 parts oil to 1 part
vinegar. You can decrease oil ratio if you substitute less tartrice
vinegar, lemon juice, or a combination of vinegar and orangeor
grapefruit juice.
You can use any canned white beans such as garbanzo,
[cannelloni beans are also known as navy beans].](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-163-320.jpg)


![154
Egg and Goat Cheese Frittata
(4 servings)
5 eggs
2 tbsp. milk
1 cup tomatoes
3 oz. cheese, goat crumbled
2 cups frozen broccoli chopped [thawed]
2 cups brown rice, cooked
Salt and pepper to taste
1. Mix eggs and milk in a large bowl. Add crumbled goat
cheese and chopped veggies and cooked rice. Season with
salt and pepper.
2. Spray muffin tin with cooking spray [Pam]. Spoon egg
mixture into muffin tins.
3. Bake at 350 degrees-15 min or until set and lightly
browned
4. Refrigerate until ready to serve-then heat in microwave
30 sec.](https://image.slidesharecdn.com/2d2e1552-de6e-4bdc-ab82-97110fc0cf25-160917112325/85/GUIDE-TO-ED-RECOVERY-2016-166-320.jpg)