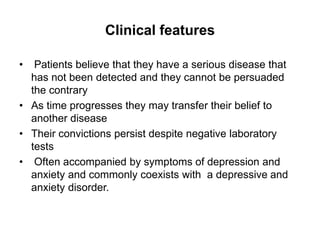
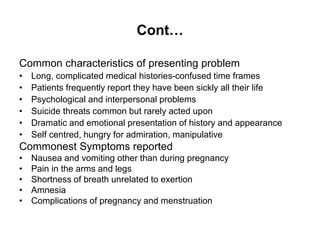
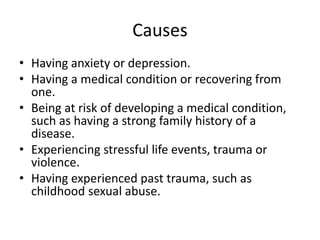
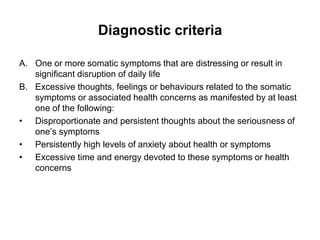
This document is a group assignment on Somatization Disorder submitted by 4 students to their professor. It includes an outline covering the introduction, clinical features, causes, diagnostic criteria, development/course, prognosis, risk factors, differential diagnosis, and treatment of Somatization Disorder. The introduction defines it as a disorder where physical symptoms are the major focus despite being medically unexplained. The clinical features section describes patients' convictions that they have an undiagnosed serious disease. Causes may include anxiety, depression, medical conditions, or stressful life events.
![Cont...
• Course modifiers:
Persistent somatic symptoms are associated with
demographic features (female sex, older age, fewer
years of education, lower socioeconomic status,
unemployment), a reported history of sexual abuse
or other childhood adversity, concurrent chronic
physical illness or psychiatric disorder (depression,
anxiety, persistent depressive disorder [dysthymia],
panic), social stress, and reinforcing social factors
such as illness benefits.](https://image.slidesharecdn.com/group2somaticdisorders-230730141149-ea868eff/85/Group-2-somatic-disorders-pptx-13-320.jpg)