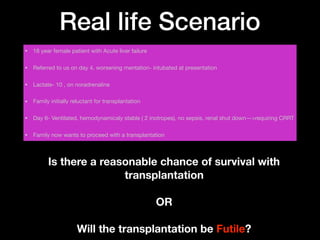
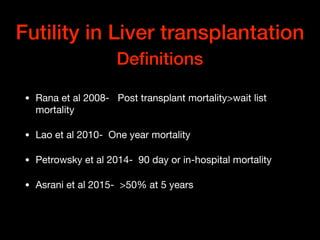
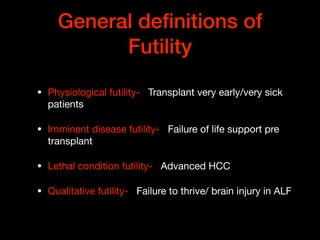
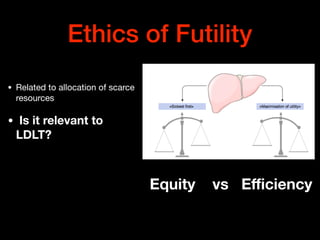
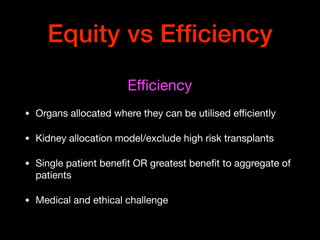
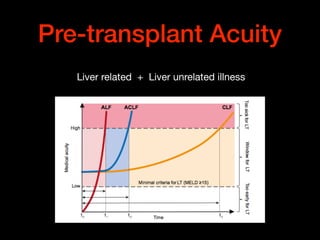
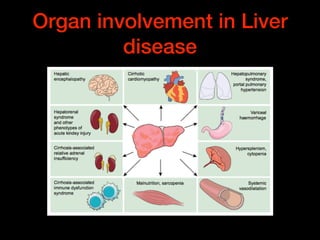
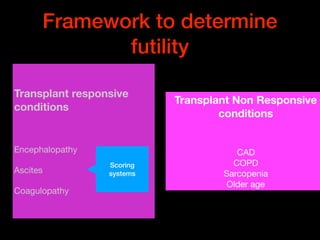
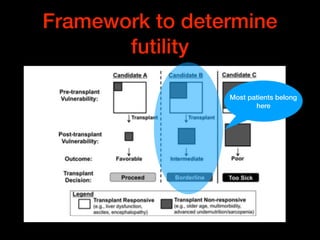
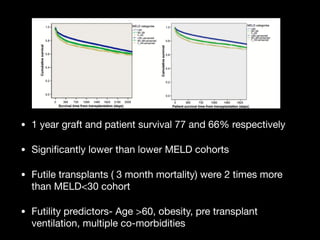
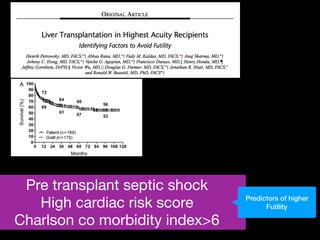
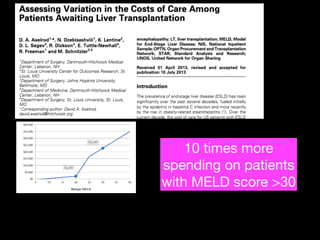
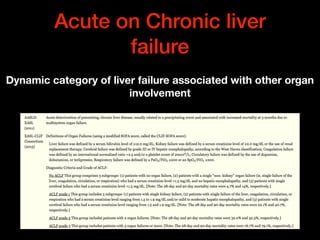
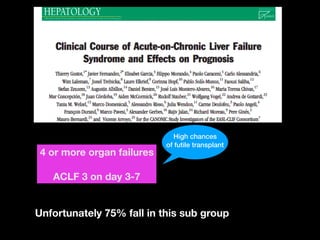
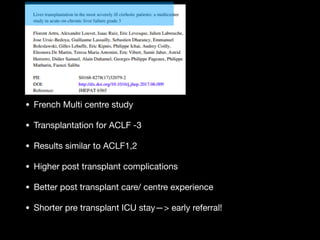
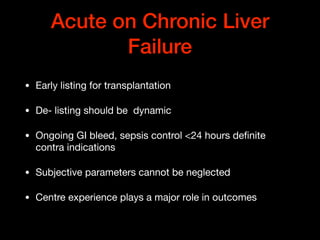
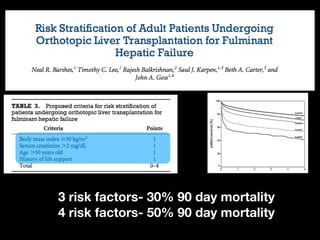
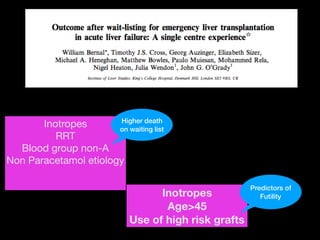
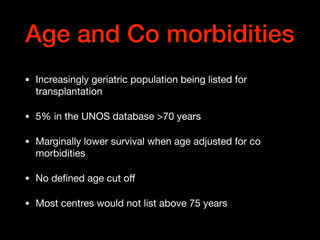
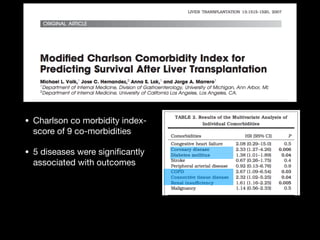
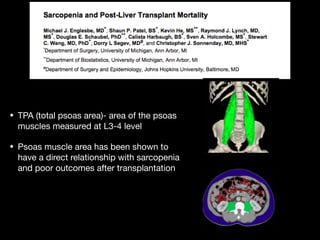
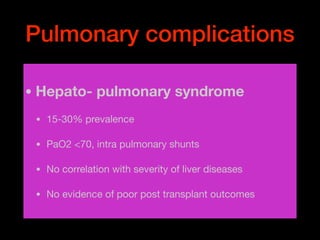
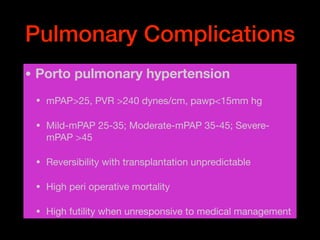
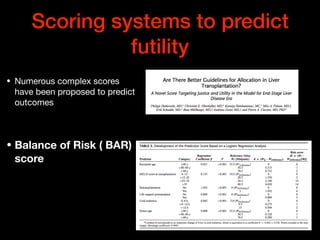
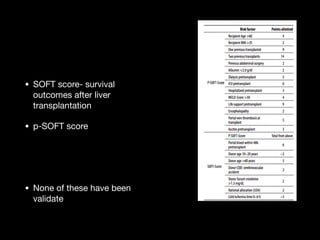
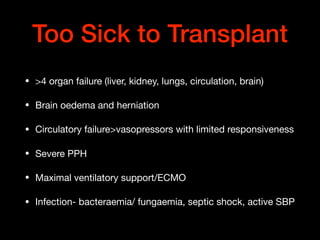
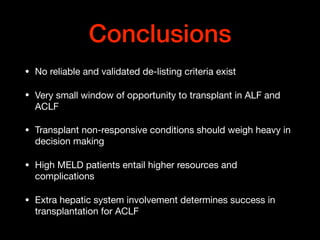
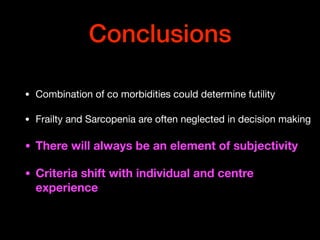
This document discusses the concept of futility in liver transplantation, focusing on various definitions and scenarios that can lead to poor outcomes post-transplant. It highlights the importance of factors such as medical acuity, organ involvement, frailty, and co-morbidities in predicting transplant futility, especially for high MELD score patients. The conclusion emphasizes the need for careful assessment and individual consideration in transplantation decisions, as well as the scarcity of reliable de-listing criteria.