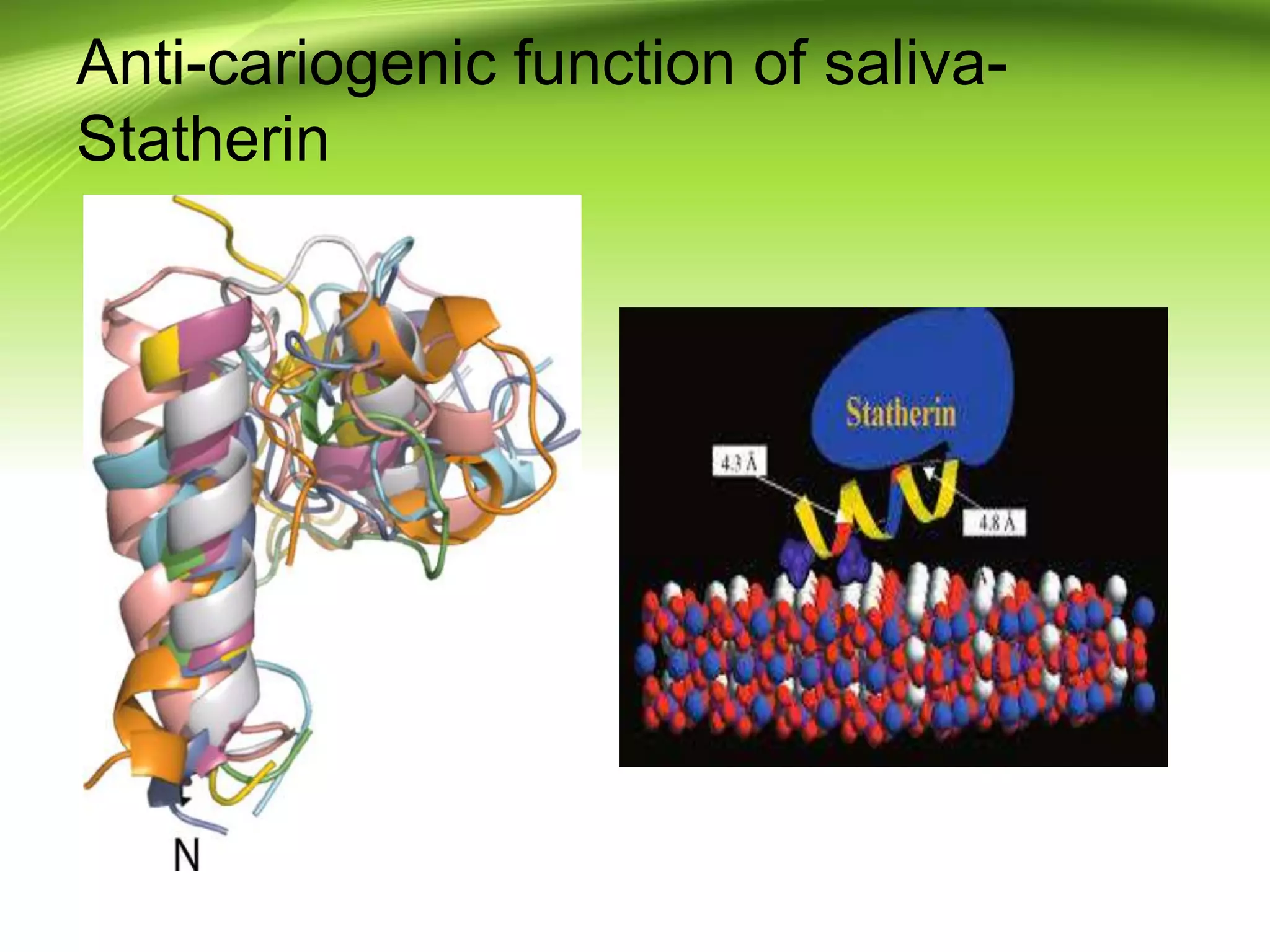
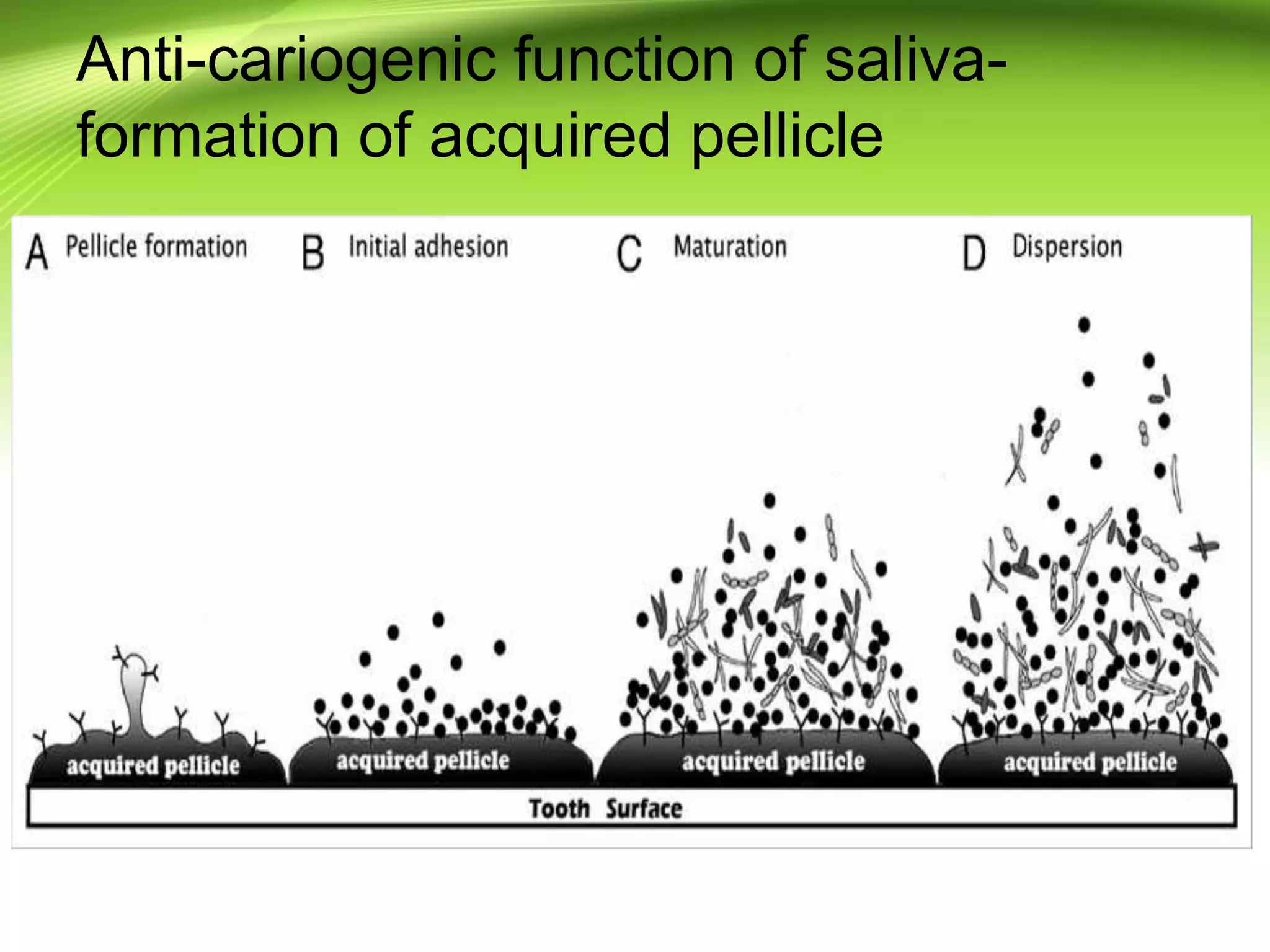
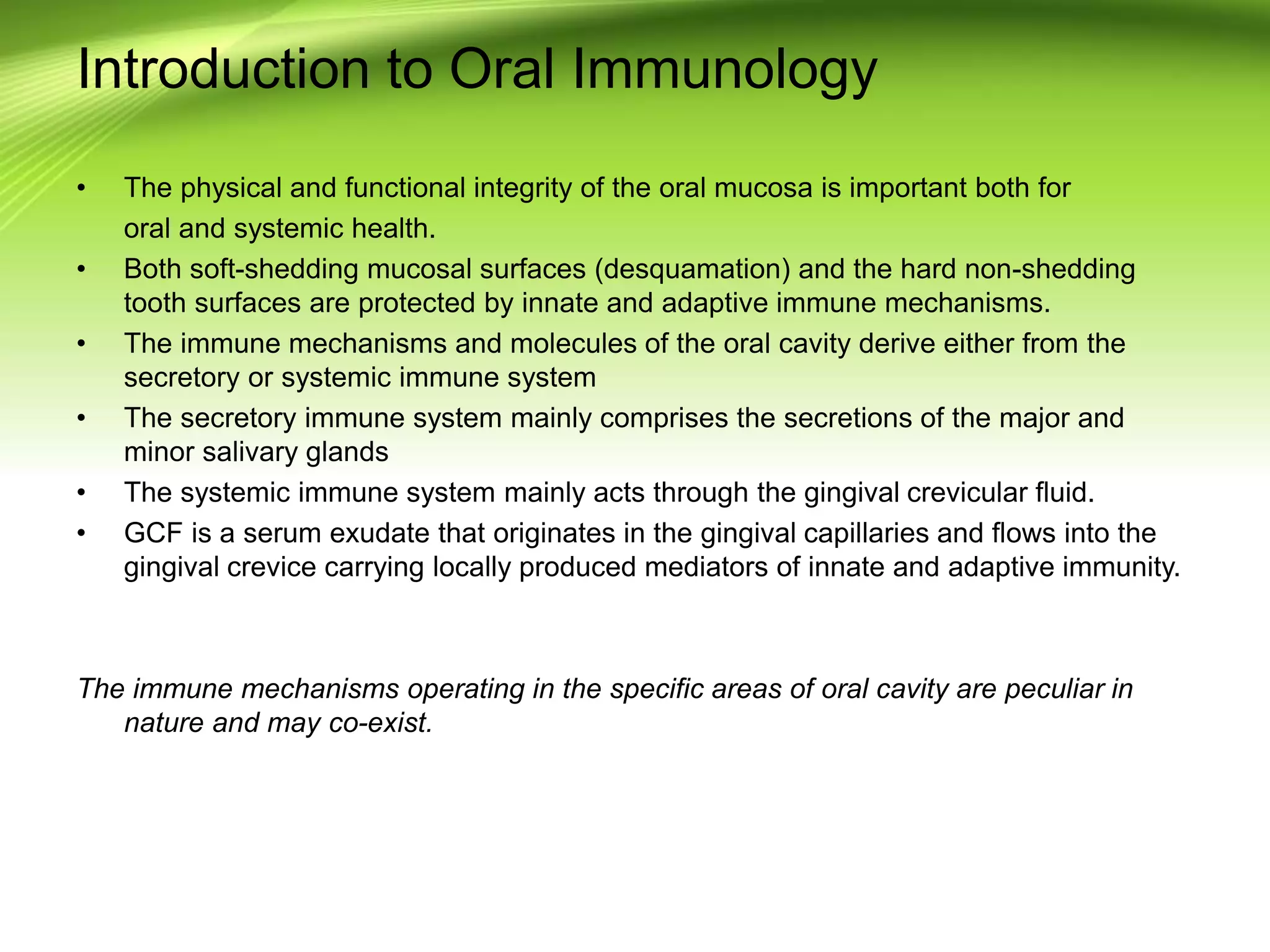
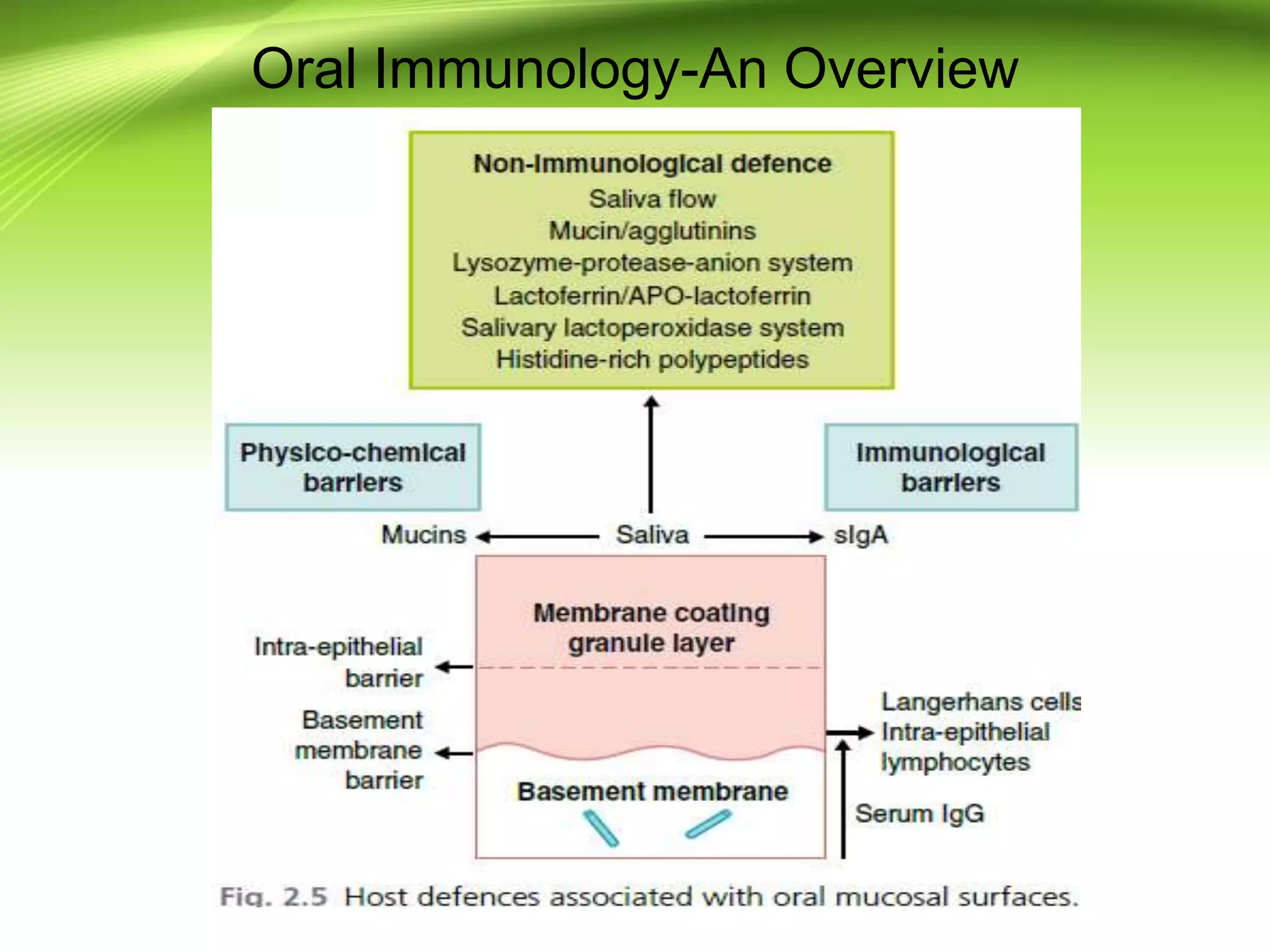
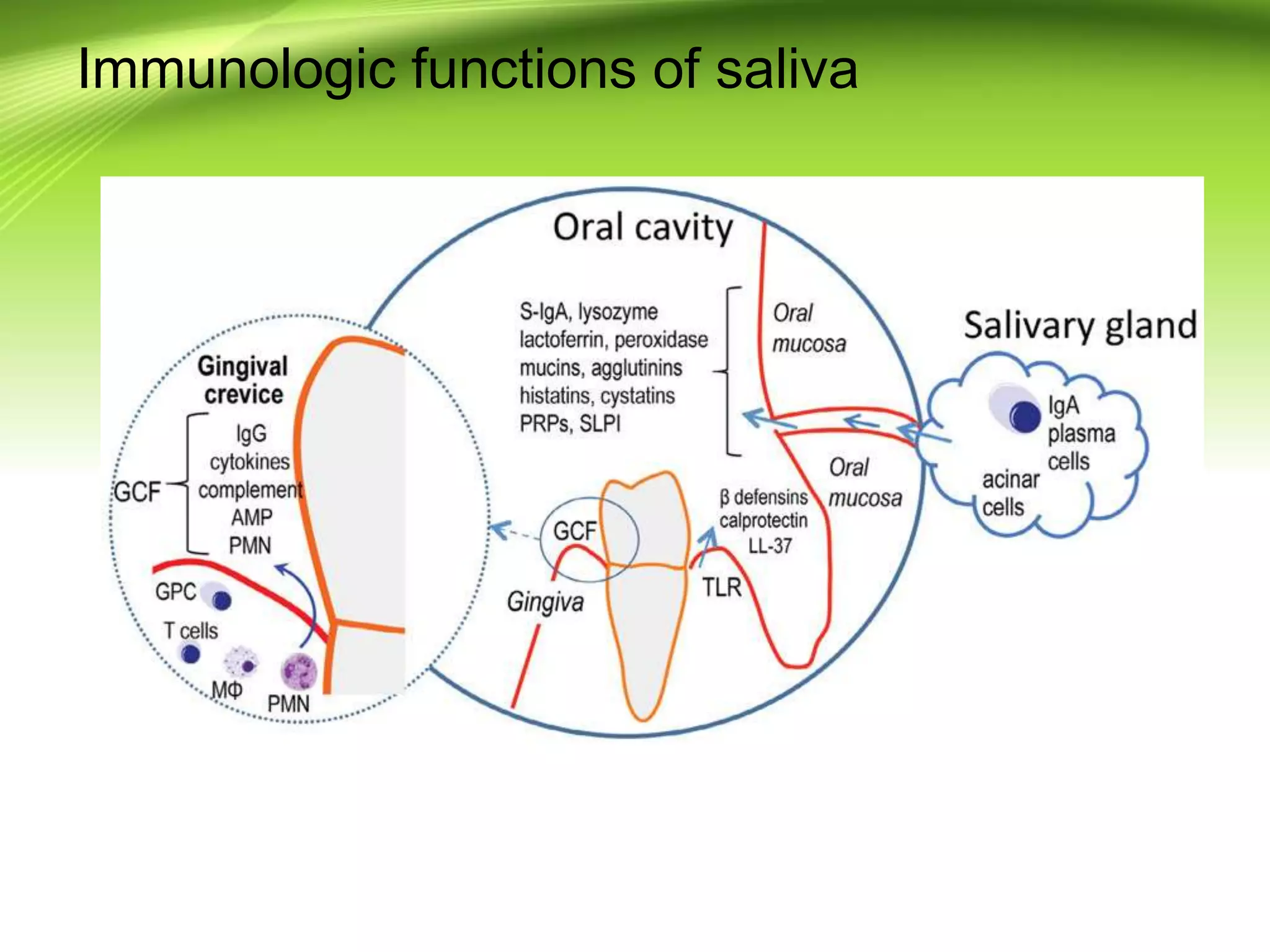
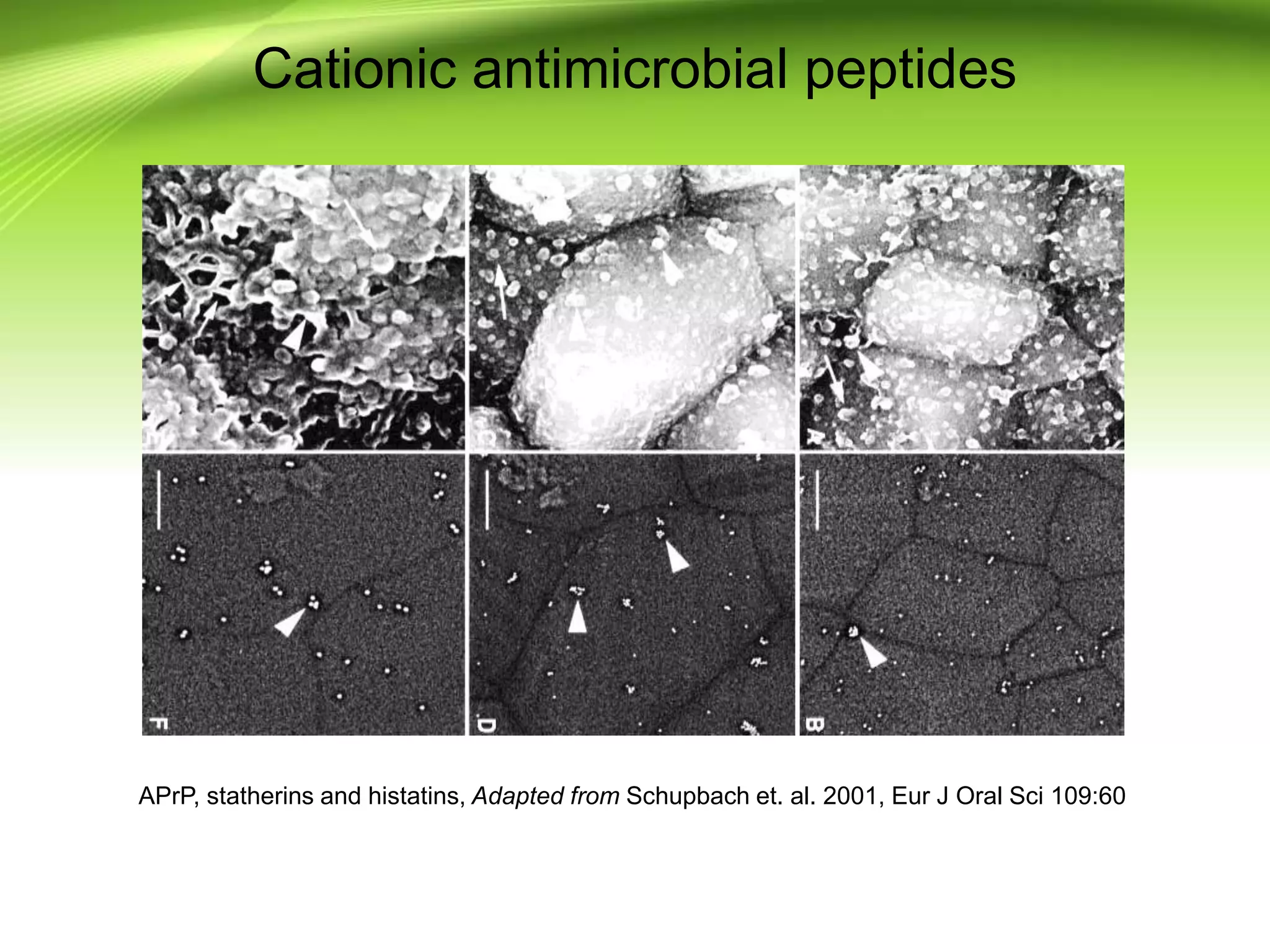
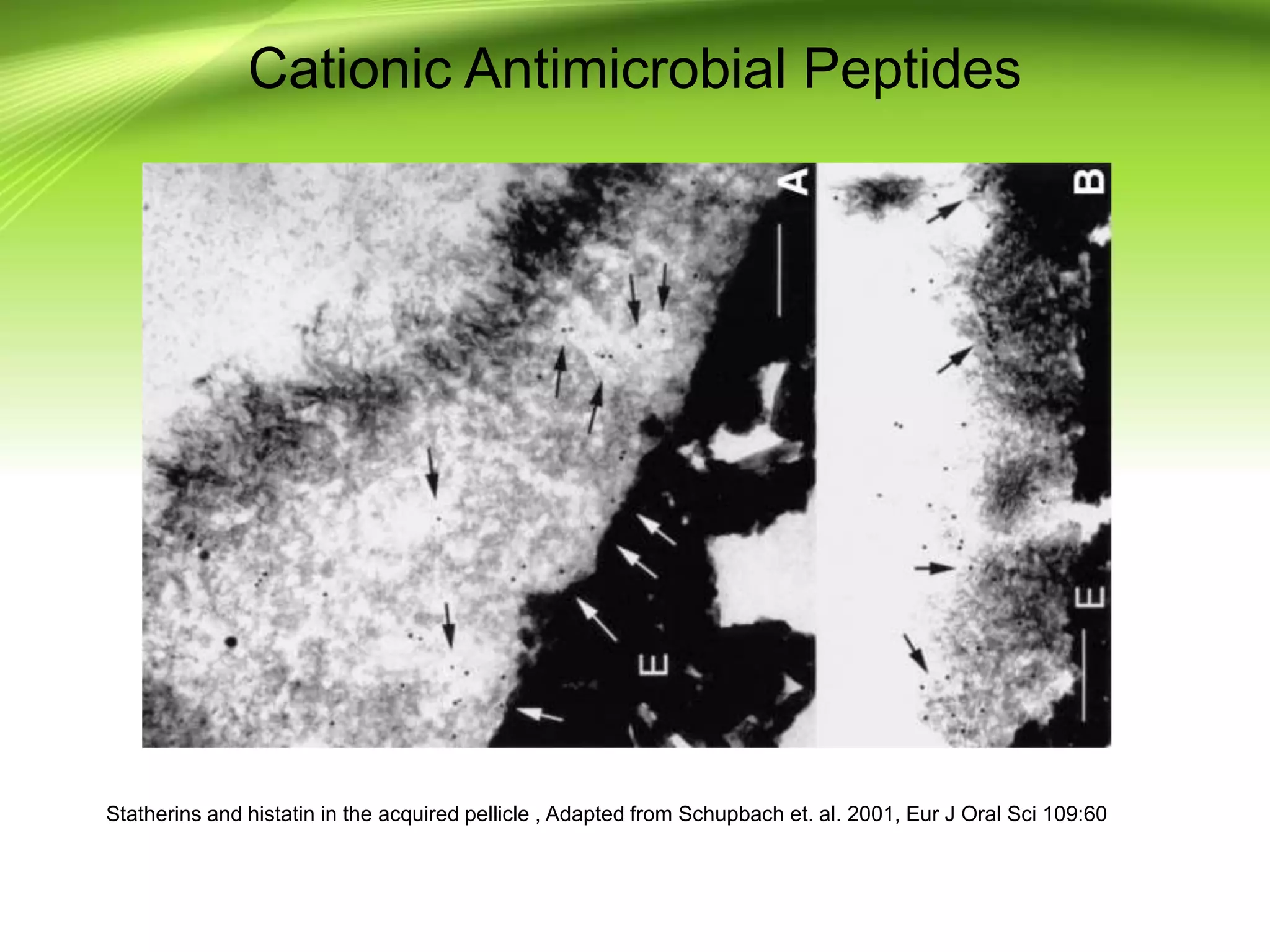
The document discusses the functions of saliva, highlighting its role in oral physiology, including the production of saliva by major and minor salivary glands, its protective and digestive functions, as well as its immunologic properties. It details the anti-cariogenic function of saliva and its components, such as statherin, which forms a protective biofilm on teeth, alongside various immune molecules that protect against oral diseases. Additionally, it explores the significance of salivary proteins and enzymes in microbial clearance and the development of innovative oral care products that leverage these properties.