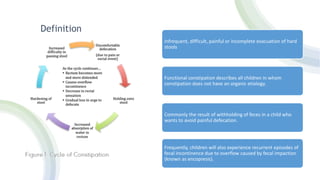
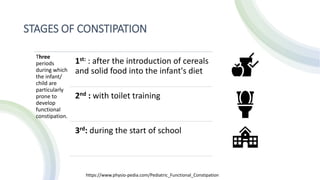
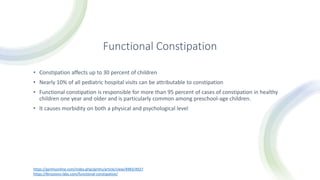
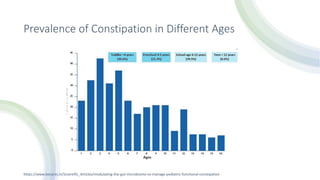
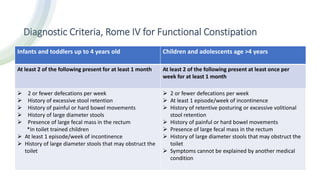
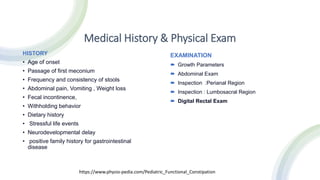
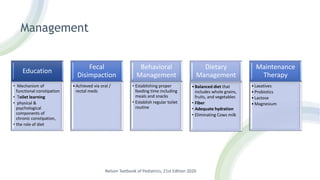
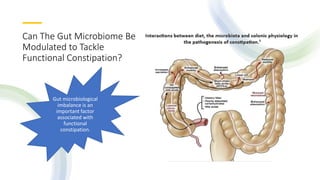
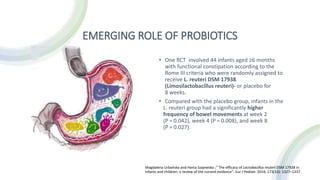
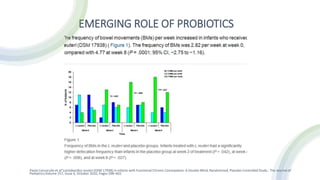
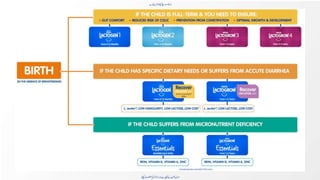
Functional constipation is a common issue in pediatric patients, affecting up to 30% of children and causing significant morbidity. The condition is characterized by infrequent or painful bowel movements and can arise from withholding behavior and various developmental stages such as dietary changes and toilet training. Management includes education, dietary modifications, and in some cases, probiotic treatments to improve symptoms.