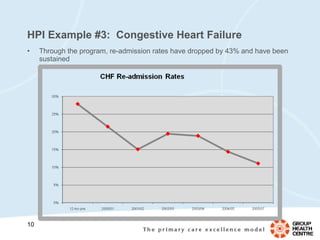
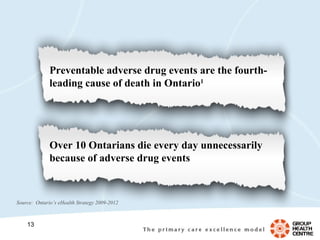
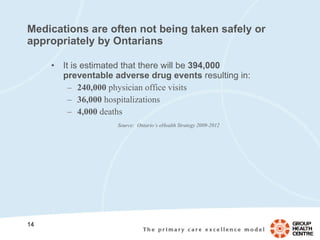
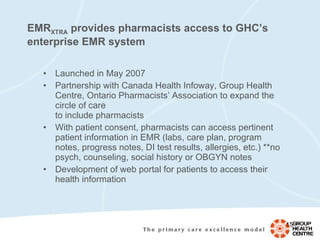
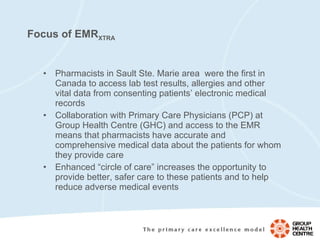
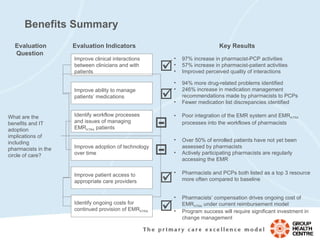
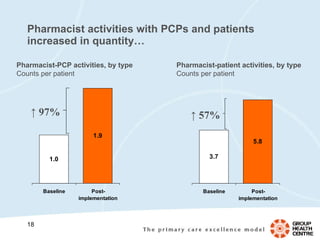
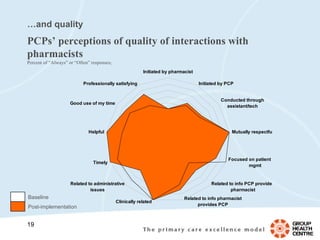
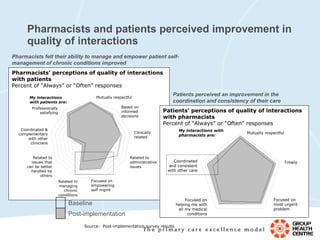
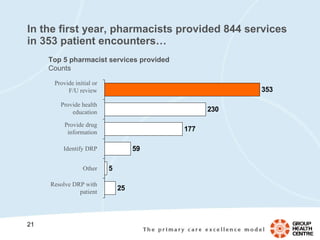
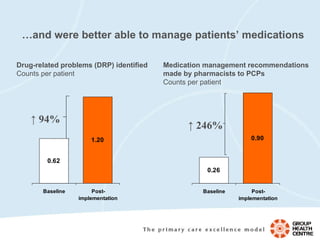
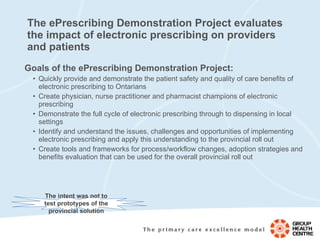
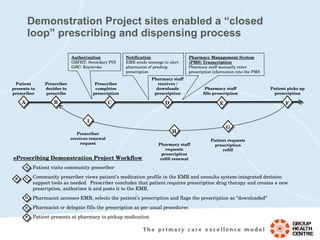
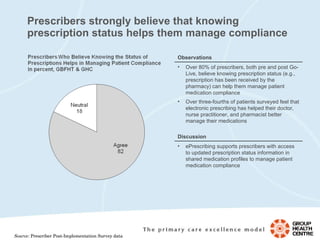
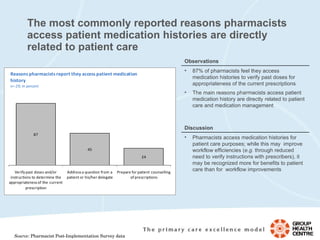
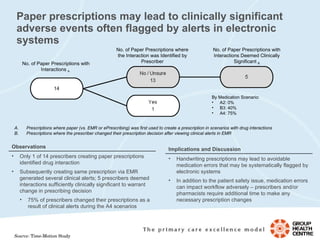
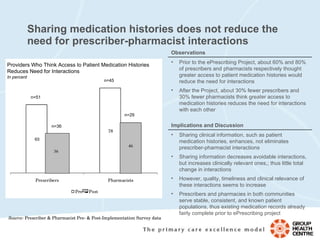
The document discusses initiatives at Group Health Centre to improve patient care through health information technology innovations. It describes the implementation of an electronic medical record system (EMR XTRA) that allows pharmacists to access patient information, increasing collaboration between pharmacists and physicians. An evaluation found the program improved quality of care by identifying more drug-related problems and increasing medication management recommendations. The document also discusses preparing for electronic prescribing (ePrescribing) to further enhance coordination and safety of patient care.

![Questions? Lucy Fronzi [email_address]](https://image.slidesharecdn.com/fronzighc-100407110020-phpapp01/85/Fronzi-Ghc-34-320.jpg)