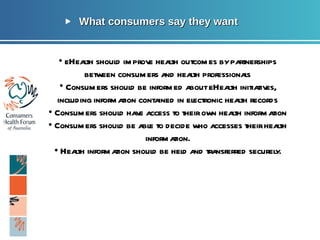
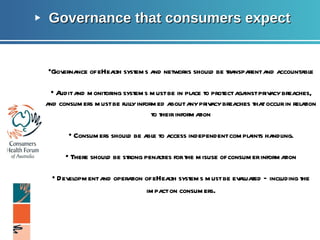
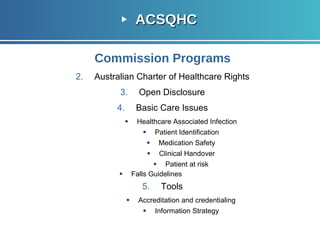
This document discusses consumers' participation in clinical handovers between general practitioners (GPs) and hospitals. It notes that currently, formal discharge summaries are only issued to GPs 10-20% of the time and specialists provide formal feedback 10-20% of the time. The document proposes that a personally controlled electronic health record (PCEHR) could help by giving patients more timely access to their clinical information and allowing for easier sharing of information between healthcare providers. This could support chronic disease management and improve healthcare quality through more coordinated team-based care.