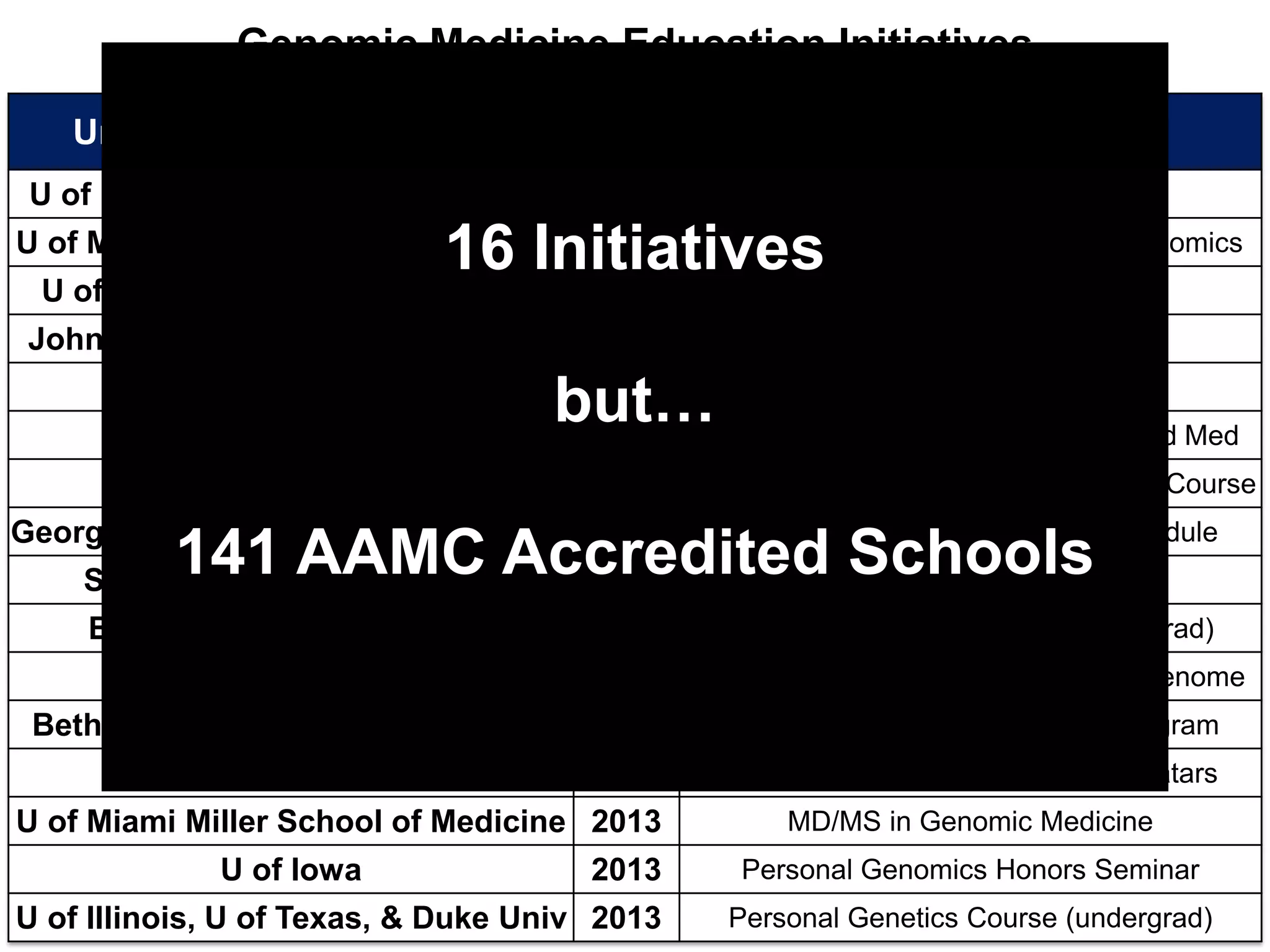
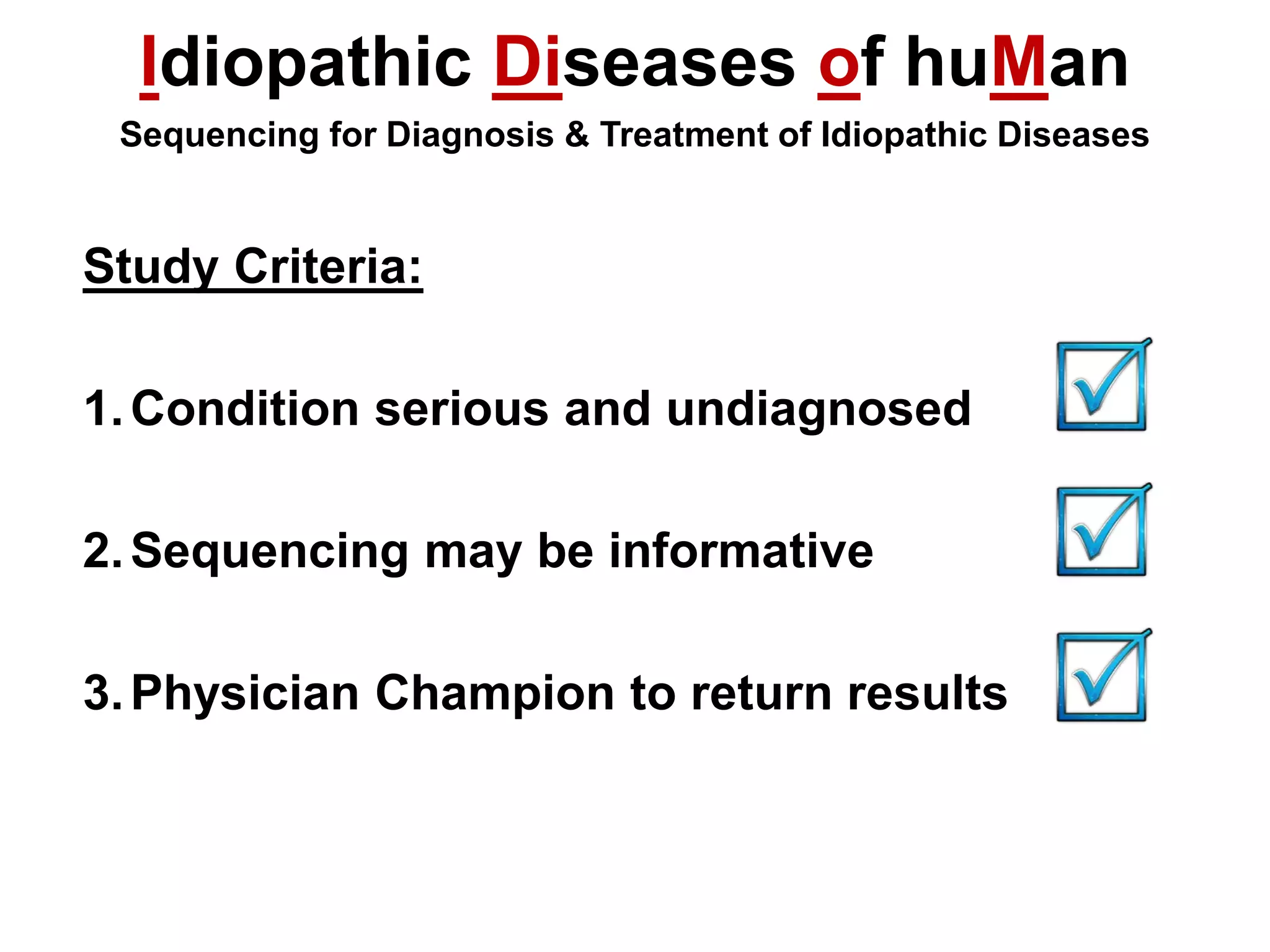
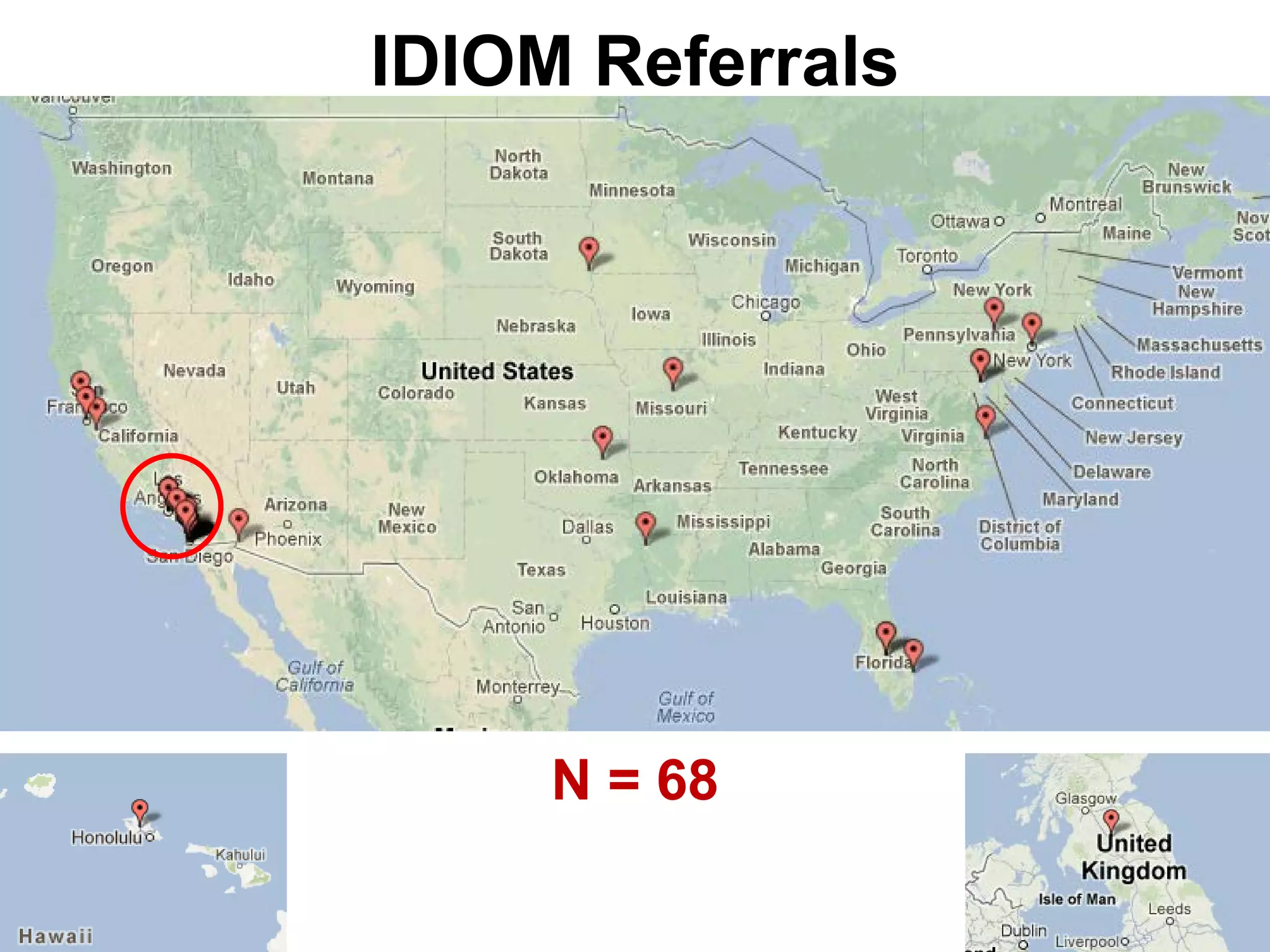
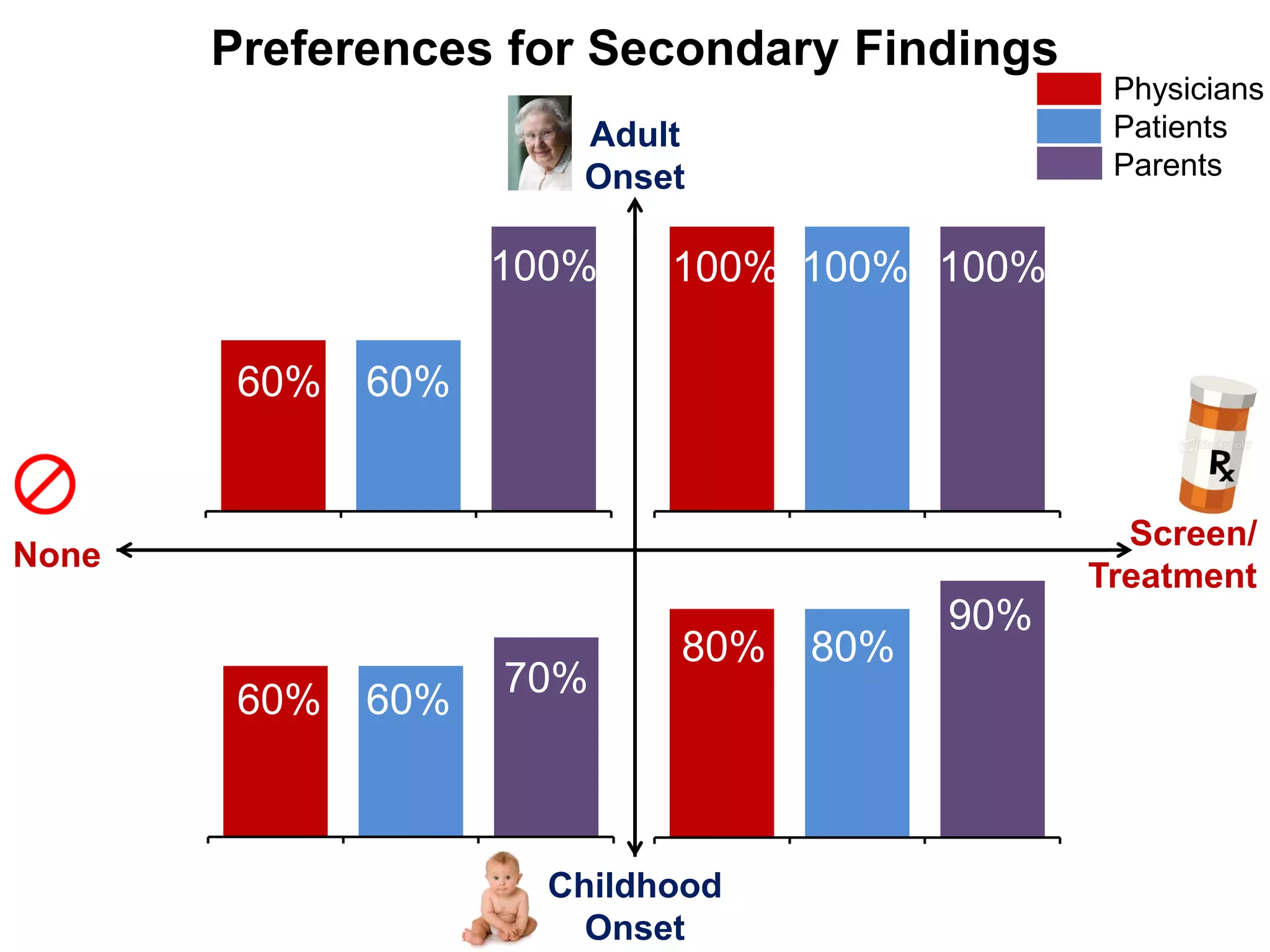
This document summarizes key findings from a study on returning genomic sequencing results to patients with idiopathic diseases and their physicians. The study found that [1] physicians may need help interpreting and communicating genomic results to patients, as post-sequencing patients graded their physician's communication skills lower than pre-sequencing, and [2] both patients and physicians preferred that secondary or incidental findings from sequencing be returned. The study highlights the challenges of integrating genomic medicine into clinical practice and the need for improved physician education in genetics and result disclosure.











![Post-Sequencing
"We took several hours post-[testing to discuss results]
which is not feasible in general practice.” - Physician Case 1
"Make it faster so it's more relevant.” - Patient Case 2
"Do not depend on [a] child's doctor to…transfer such
important information.” - Father Case 3
• Mild to no sequencing-related distress, little to no regret
• 75% physicians & 50% patients suggest added clinician](https://image.slidesharecdn.com/fogm-vicinnamonblossidiom7march2013finalpost-130308080332-phpapp01/75/Fo-gm-vi-cinnamonbloss_idiom_7march2013_fina_lpost-17-2048.jpg)