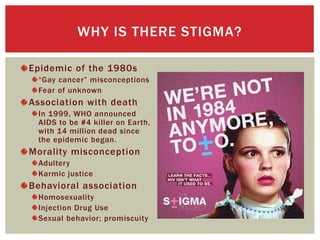
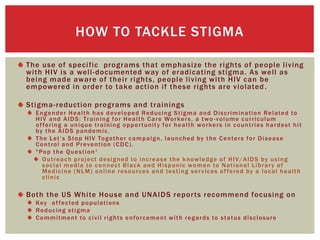
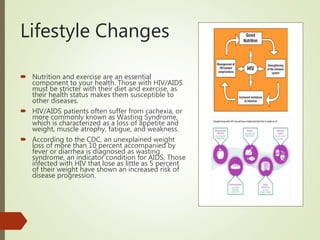
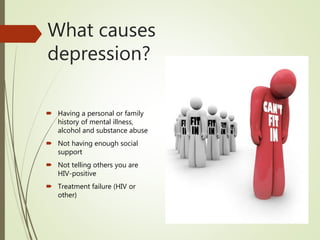
The document provides guidance for individuals diagnosed with HIV/AIDS on how to live with their diagnosis. It discusses the need for lifestyle changes like improved nutrition, exercise and safer sex practices. It also emphasizes the importance of communicating one's status to close relationships and seeking counseling to cope with potential depression and stigma. Support groups and healthcare services are recommended to help patients manage their condition and quality of life.