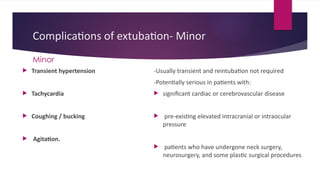
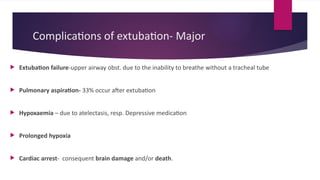
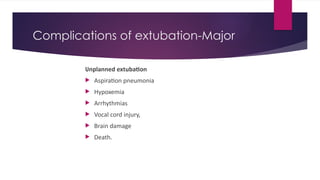
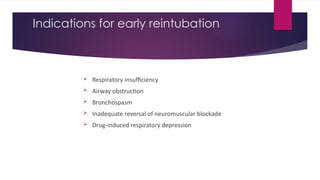
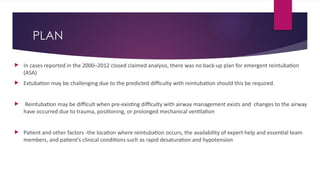
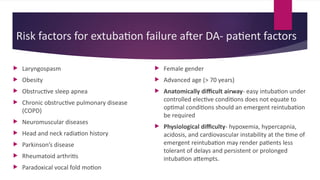
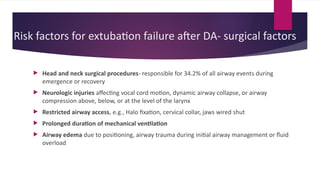
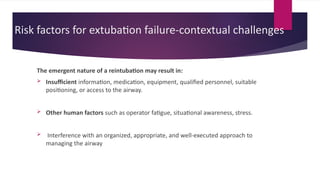
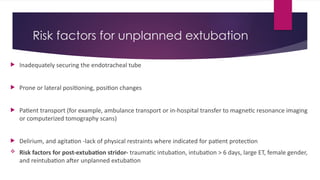
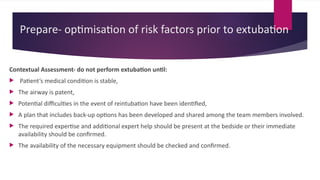
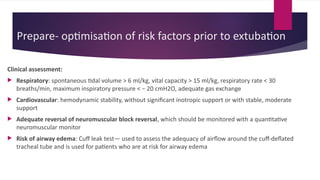
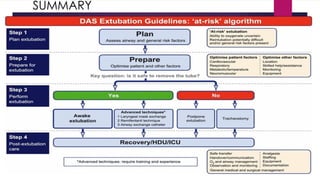
The document discusses the risks and techniques associated with extubation of difficult airways, emphasizing the importance of careful planning and execution. It outlines potential complications of extubation, including both minor and major issues, as well as risk factors contributing to extubation failure. Established guidelines like the 4Ps of extubation are provided to enhance safety during this critical procedure.