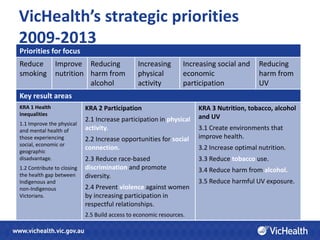
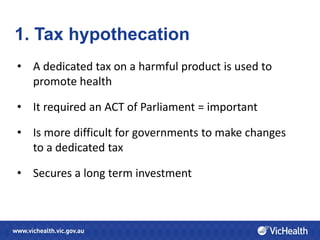
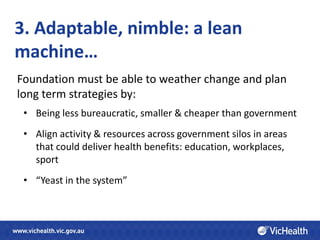
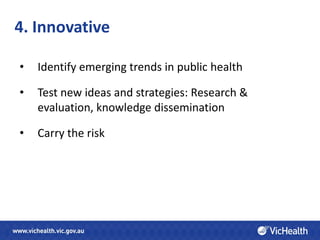
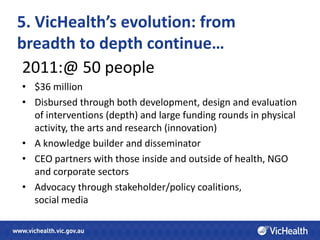
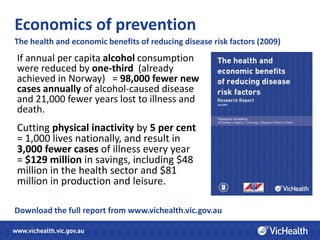
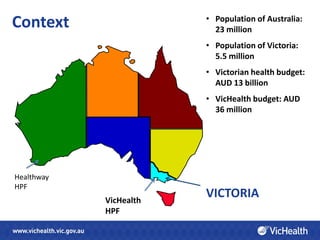
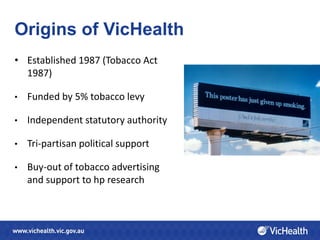
VicHealth is a health promotion foundation established in Victoria, Australia in 1987 using funds from a 5% tobacco tax levy. It has evolved from broadly distributing funds to focusing on in-depth interventions and knowledge building. Key lessons include establishing an independent statutory authority through dedicated taxation; adapting to change through a lean structure; testing innovative strategies; and building cross-sectoral partnerships. VicHealth works across settings like education, workplaces and sports to address priorities like reducing smoking, improving nutrition and mental wellbeing. Evaluations show its efforts can significantly improve health outcomes and save costs associated with chronic diseases.


![“This ends the debate decisively.
Health care is an important
determinant of health.
Lifestyles are important
determinants of health.
But it is factors in the social
environment that determine
access to health services and
influence lifestyle choices in
the first place.”
[Source] www.who.int/social_determinants](https://image.slidesharecdn.com/experienceandlessons-ireneverins-120517040415-phpapp01/85/Experience-and-lessons-Irene-Verins-10-320.jpg)