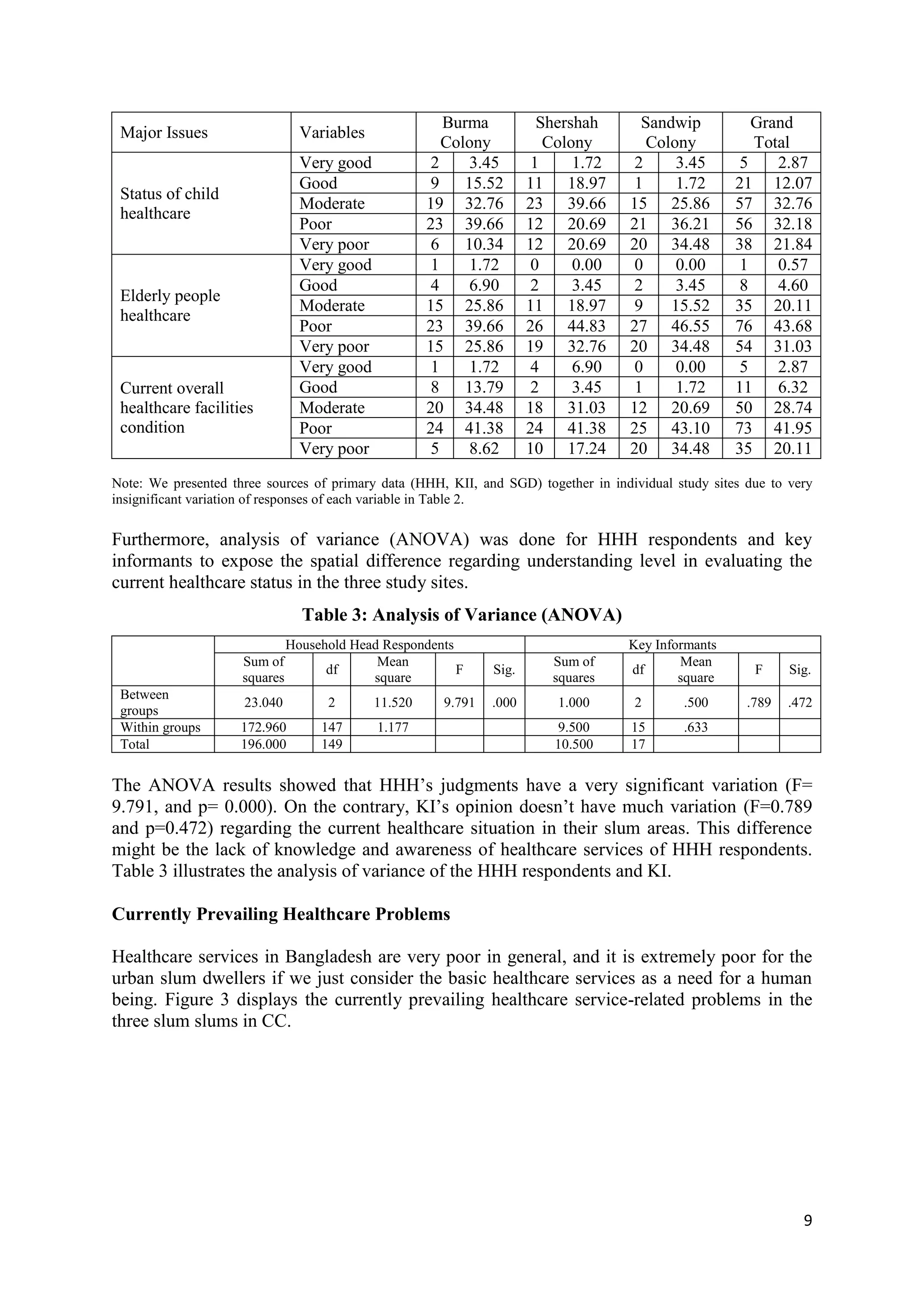
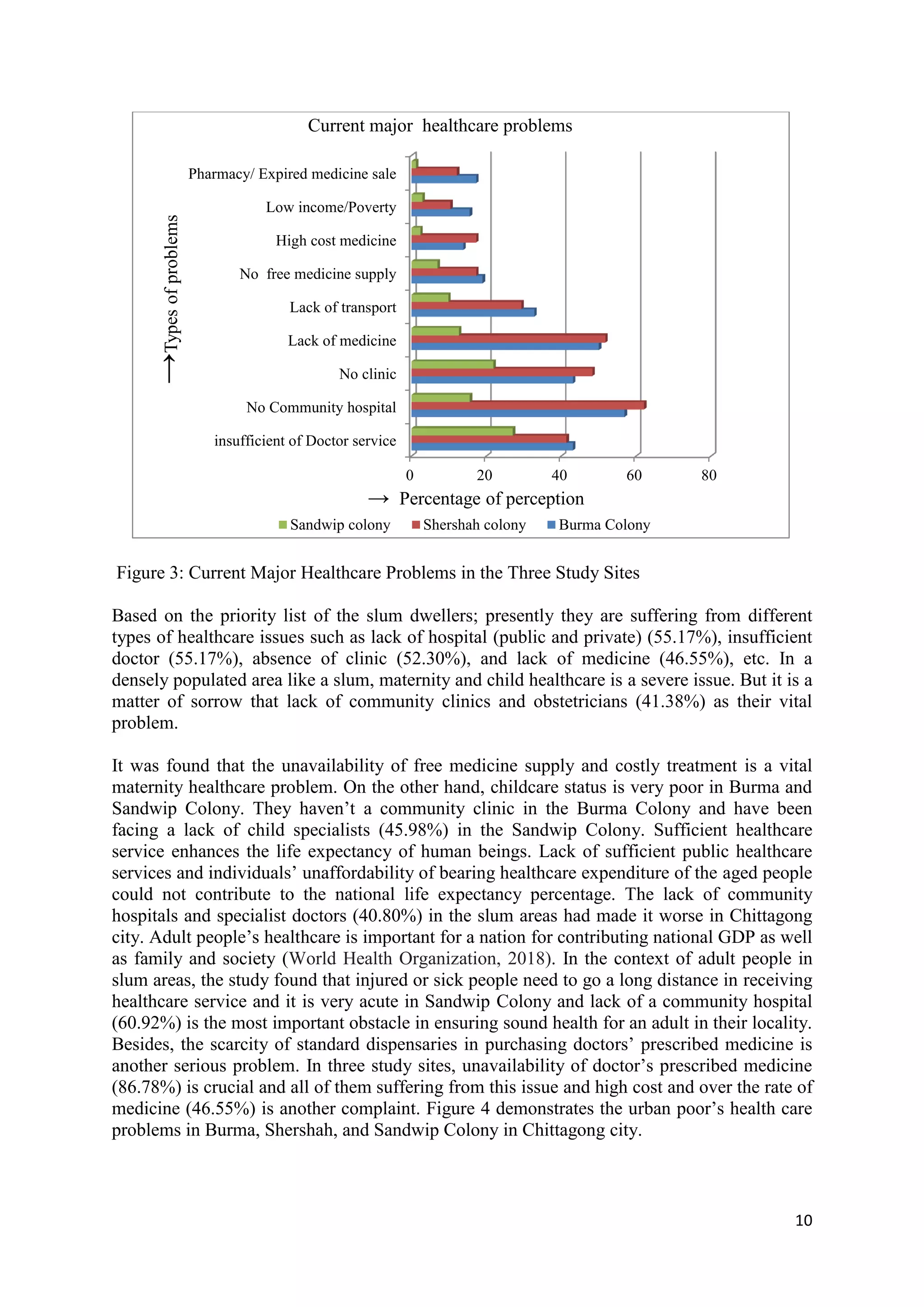
The document discusses the healthcare status and challenges faced by urban poor populations in Chittagong City, Bangladesh. It finds that overall healthcare access is moderate to very poor, especially in Sandwip Colony, due to a lack of public healthcare services and facilities like community hospitals and clinics. Establishing more accessible community healthcare facilities that provide free treatment and specialist doctors could help address issues around maternal, child, and general healthcare access for the urban poor. Further policy reforms and structural improvements are still needed to strengthen urban poor populations' access to essential healthcare services in Chittagong City.