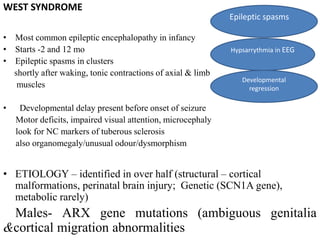
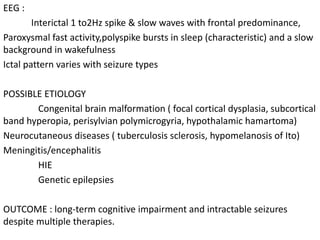
This document discusses several epileptic encephalopathy syndromes that occur in childhood. It defines epileptic encephalopathies as heterogeneous brain disorders occurring during development where abnormal EEG activity is responsible for cognitive and motor regression beyond what would be expected from the underlying etiology alone. It then describes several recognized epileptic encephalopathy syndromes in children including Ohtahara syndrome, early myoclonic encephalopathy, West syndrome, Dravet syndrome, Lennox-Gastaut syndrome, epileptic encephalopathy with continuous spike and wave during sleep, and Landau-Kleffner syndrome. For each syndrome, it provides details on age of onset, common seizure types and EEG patterns, potential etiologies,