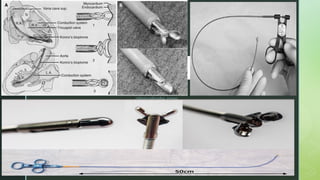
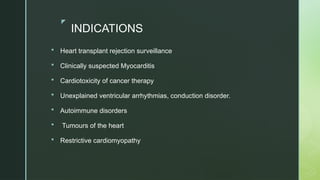
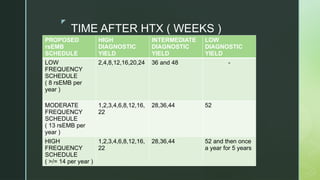
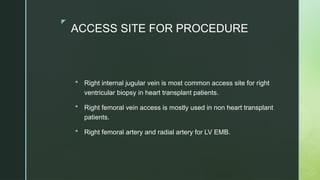
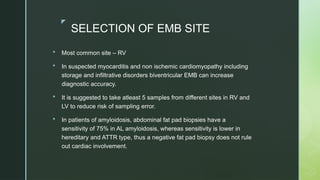
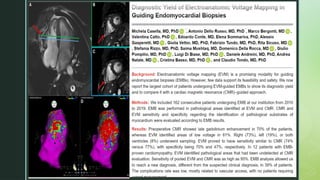
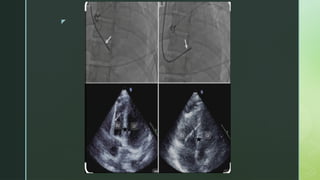
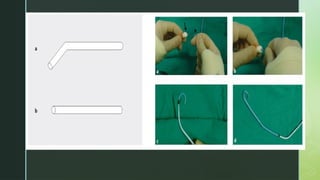
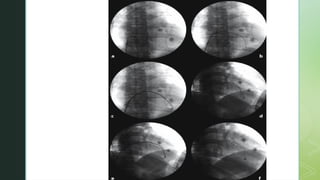
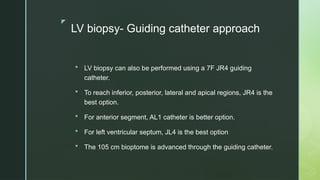
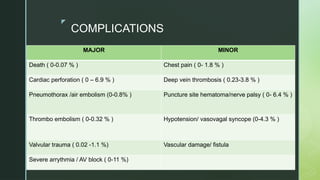
Endomyocardial biopsy (EMB) is a key invasive procedure primarily used for heart transplant rejection surveillance and diagnosing myocarditis among other conditions. The document details the historical development, techniques, indications, imaging guidance, and potential complications associated with EMB, emphasizing the procedural approaches via different vascular sites, including the right internal jugular and femoral veins. It also outlines the importance of sampling multiple sites to reduce diagnostic errors and highlights the low complication rates but notes specific risks associated with patient factors.