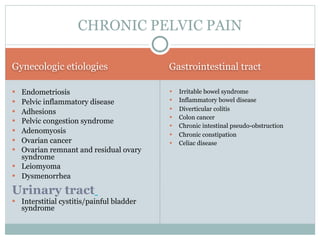
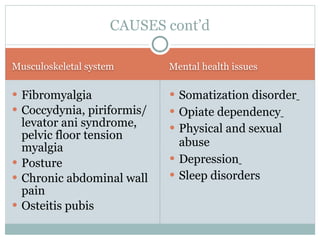
Chronic pelvic pain can have many causes, both gynecological and non-gynecological. Endometriosis, where endometrial-like tissue grows outside the uterus, is a common cause of pelvic pain among women. Theories about the etiology of endometriosis include retrograde menstruation and factors related to estrogen levels. Symptoms include dysmenorrhea, chronic pelvic pain, and dyspareunia. Diagnosis requires a histologic examination. Treatment options include medications and surgery, though medical therapy does not eradicate lesions and recurrence after surgery is common.