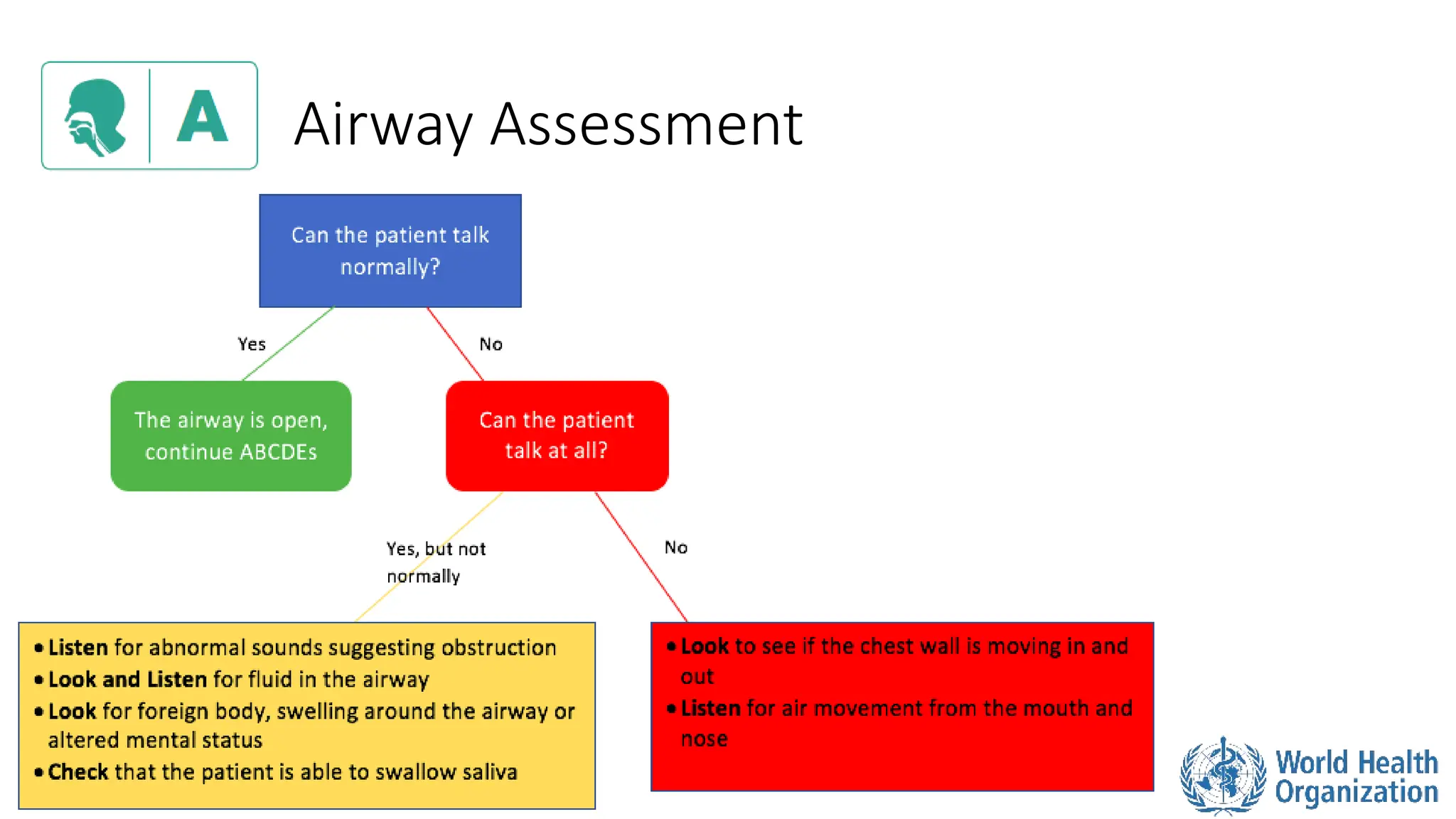
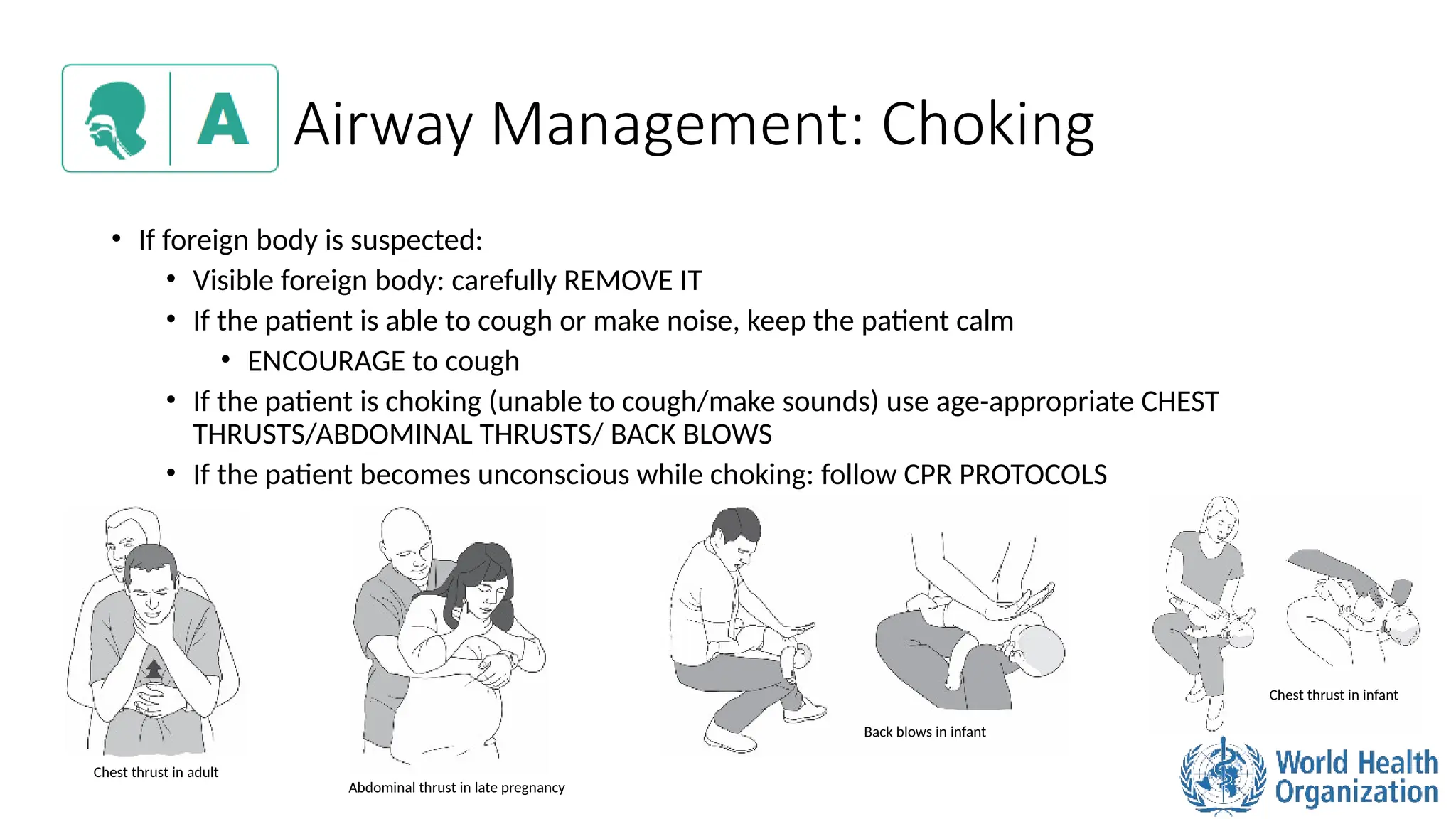
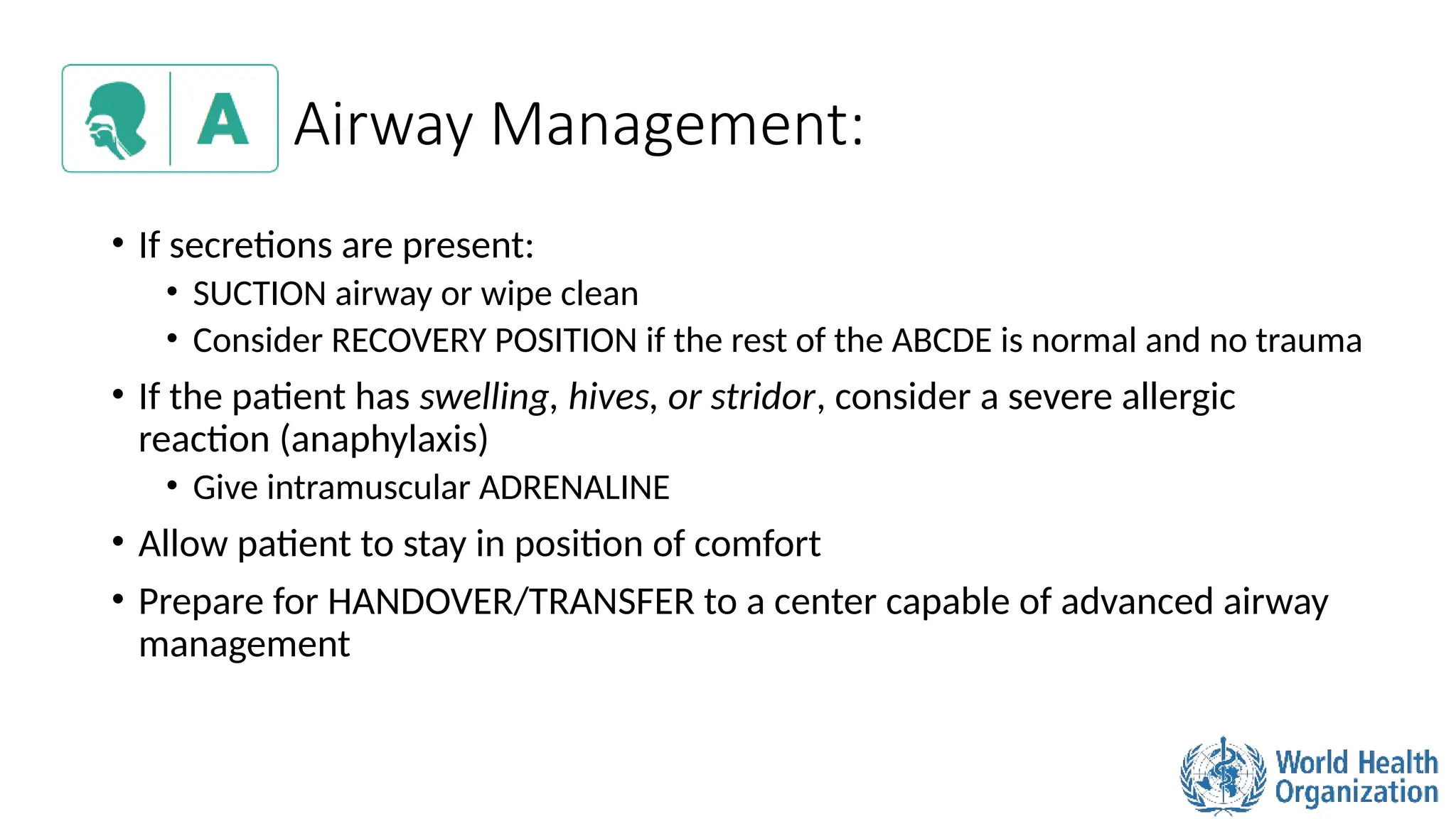
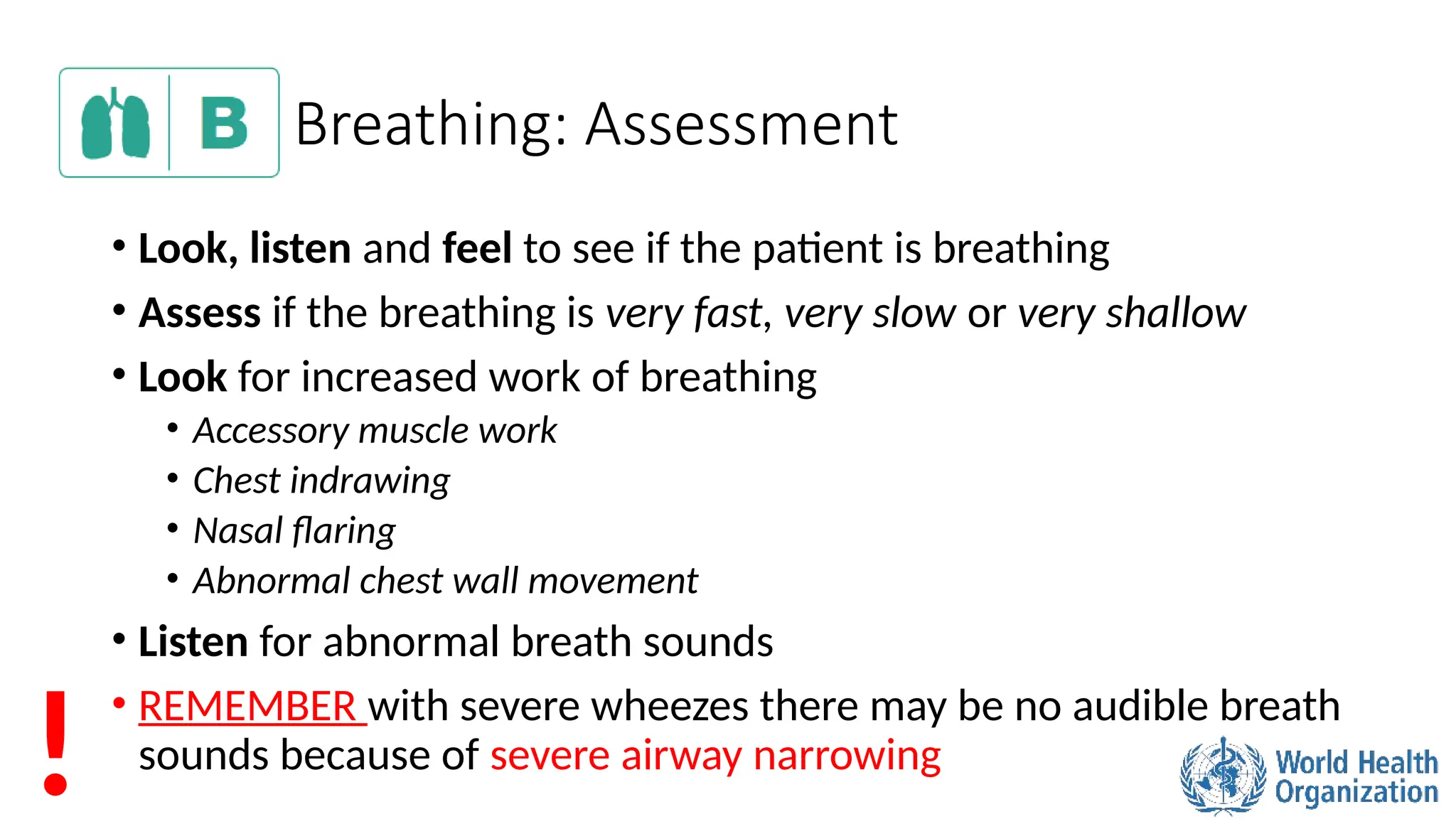
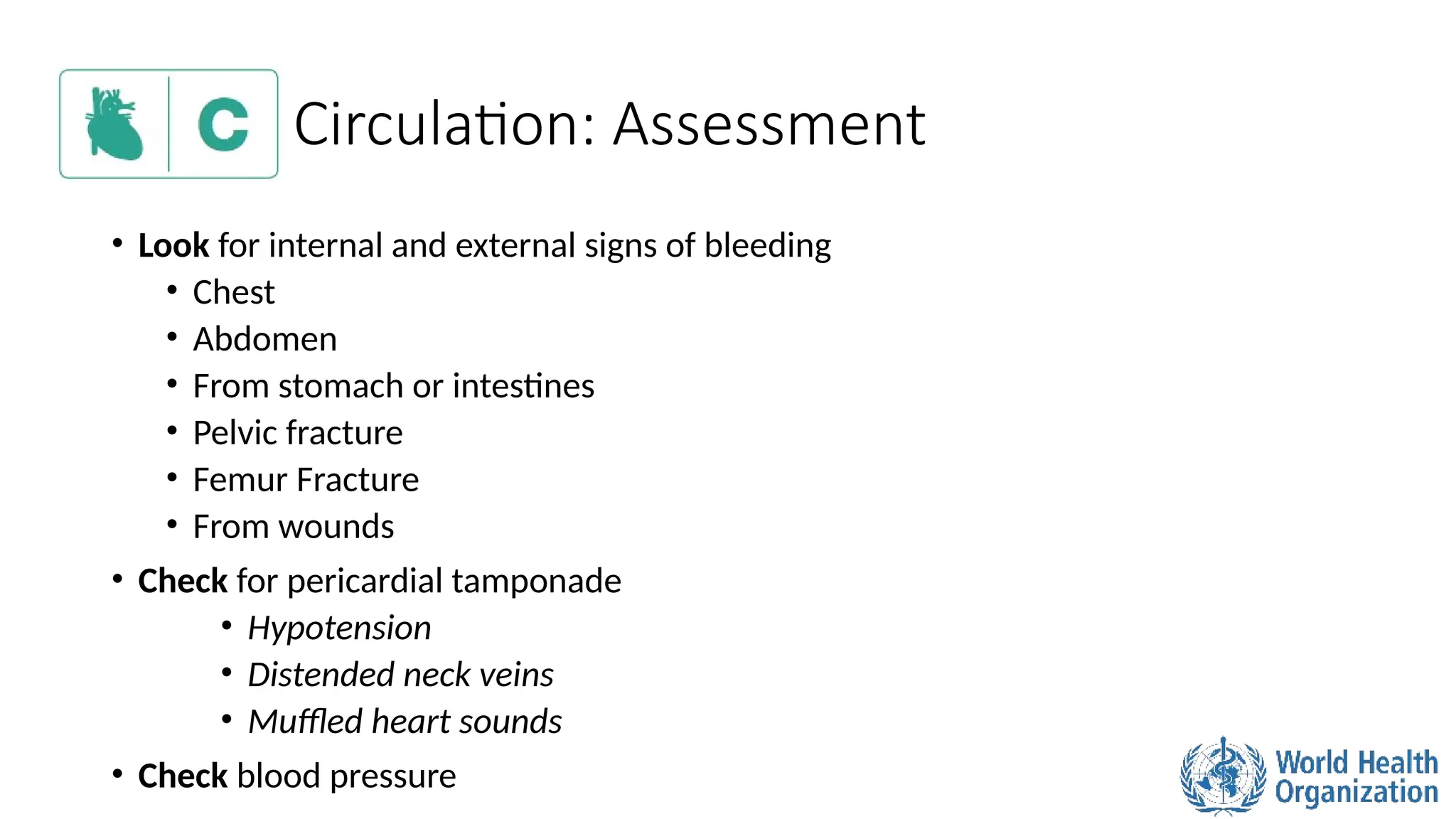
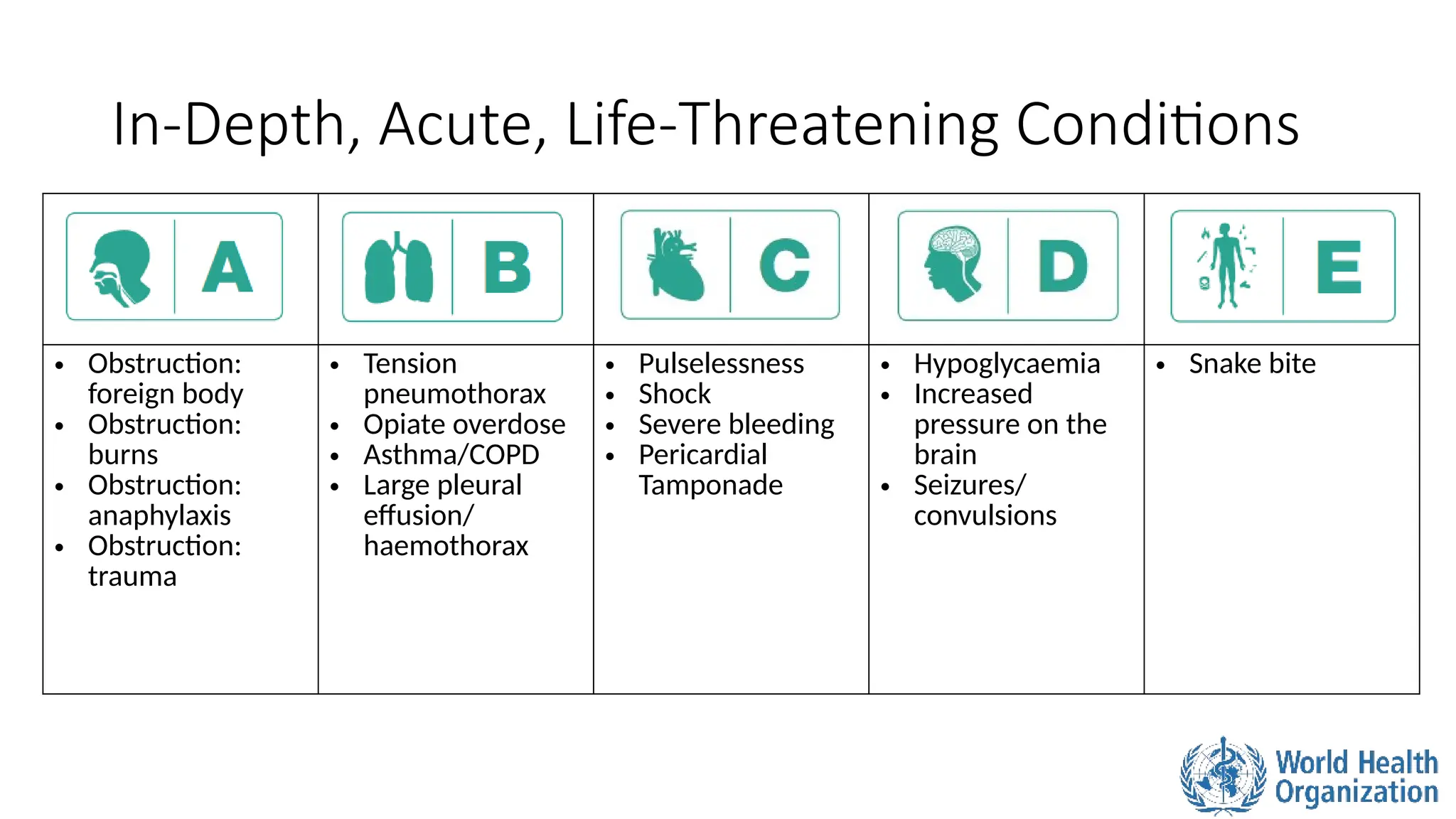
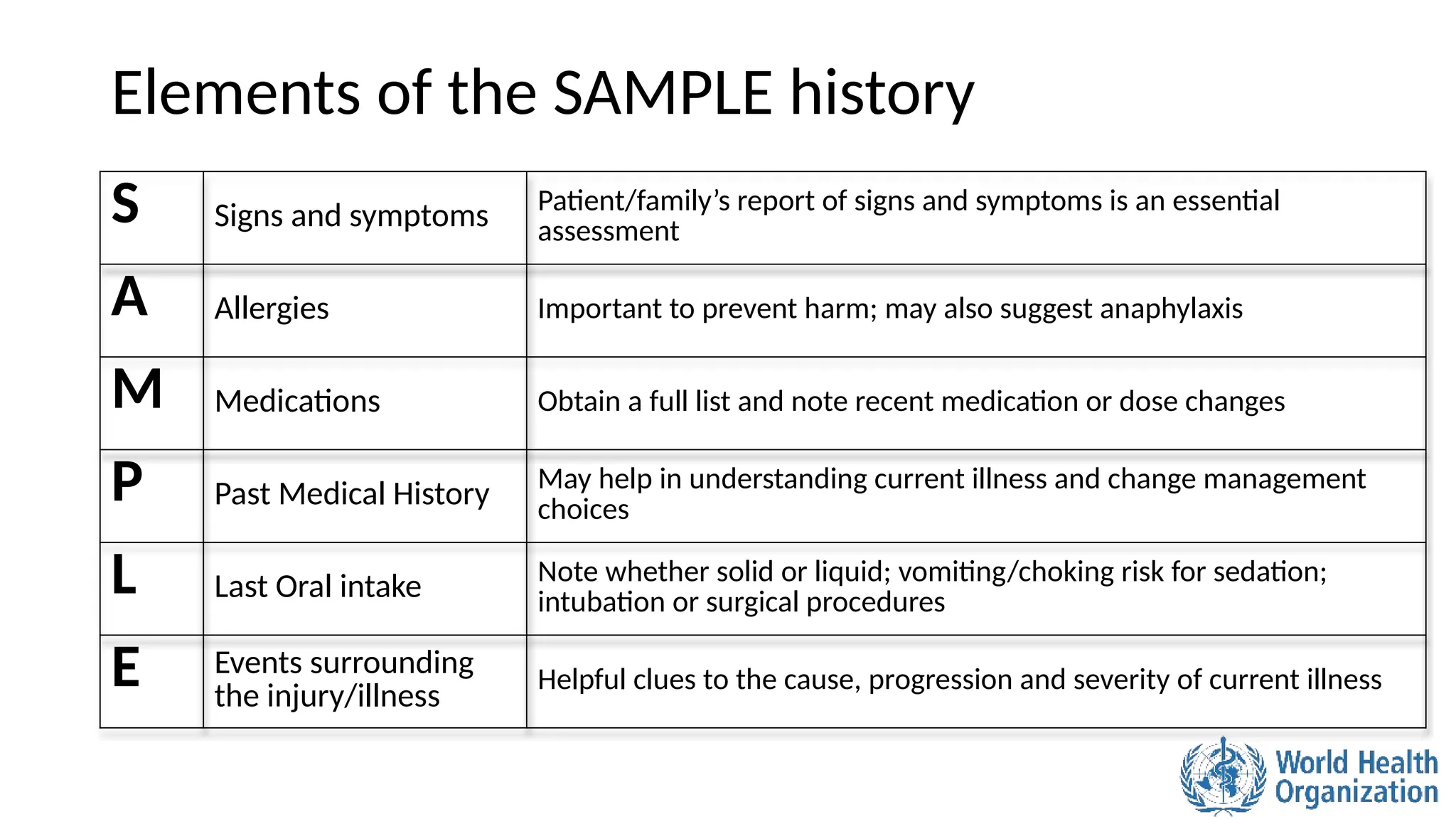
The ABCDE approach is a systematic method for the rapid assessment and management of acutely ill patients, focusing on prioritizing life-threatening conditions. Key elements include assessing Airway, Breathing, Circulation, Disability, and Exposure, while ensuring the safety of both the patient and healthcare provider. This approach emphasizes immediate identification and treatment of critical issues, as well as thorough history-taking to inform medical decisions.