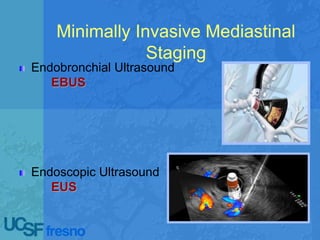
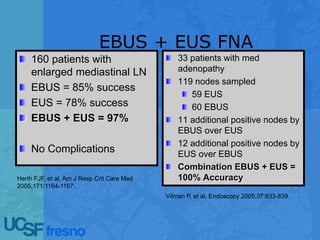
Echoendoscopic lymph node staging in lung cancer provides an endoscopic alternative to surgical staging that is minimally invasive, accurate, and prevents unnecessary surgeries. Combined endobronchial ultrasound and endoscopic ultrasound (EBUS/EUS) procedures sample lymph nodes and detect metastasis with a sensitivity of 91% and specificity of 96%, outperforming surgical staging. EBUS/EUS is now considered the new gold standard for mediastinal staging as it is safer, less costly, and more comprehensive than surgical staging alone.