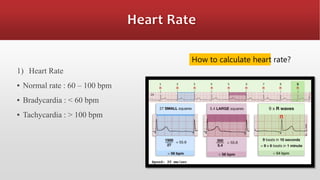
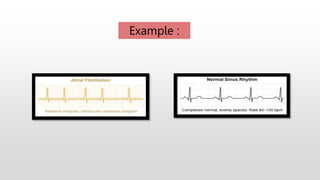
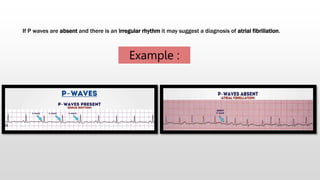
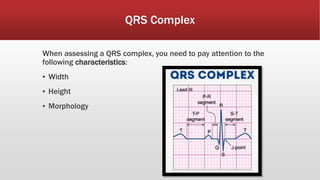
This document provides details on a case of a 51-year-old female patient presenting with diabetic ketoacidosis and atrial fibrillation. Key findings include a blood glucose of 30.7 mmol/L, ECG showing narrow complex tachycardia of 188 bpm, and lab results consistent with DKA including serum ketones of 2.4 and anion gap metabolic acidosis. Treatment involved IV fluids, insulin, antibiotics, amiodarone to cardiovert the atrial fibrillation, and monitoring until the patient was stabilized for transfer.