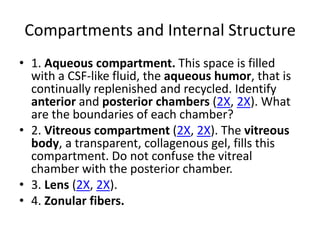
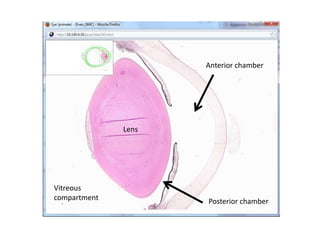
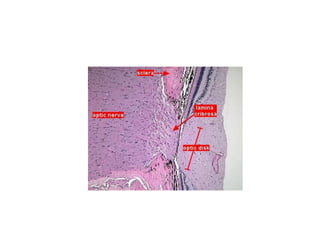
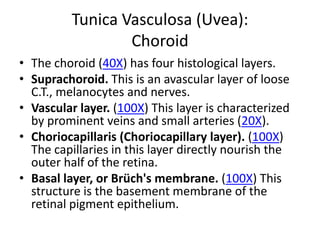
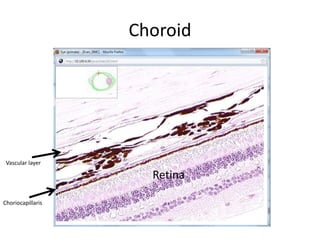
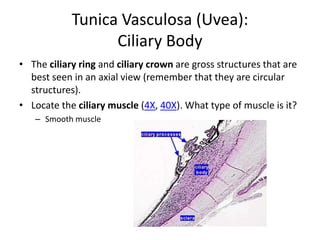
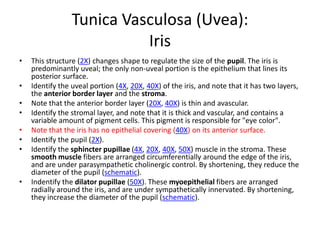
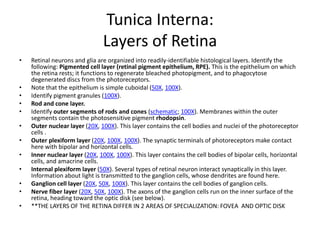
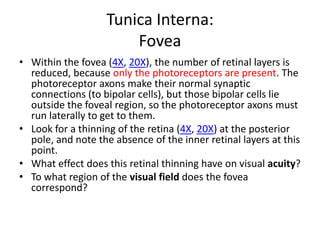
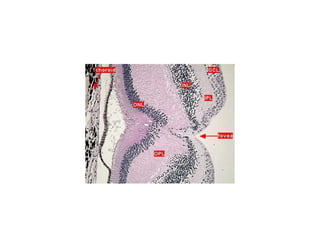
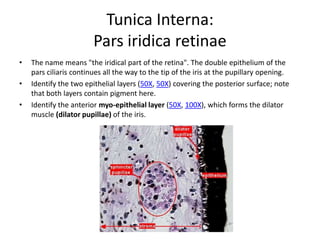
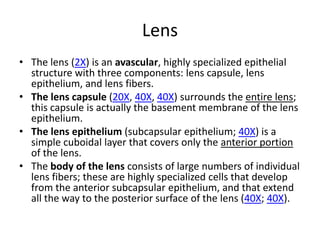
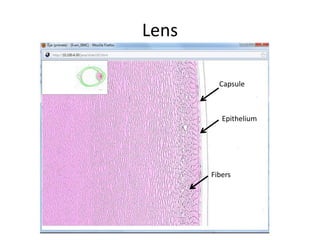
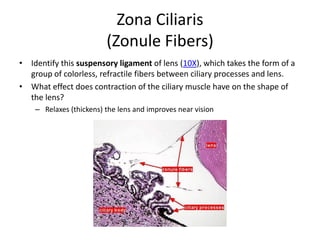
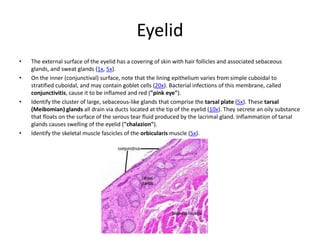
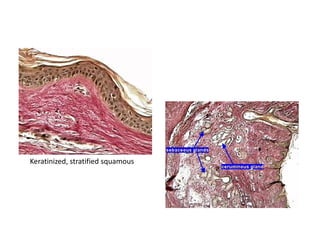
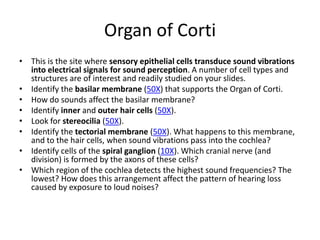
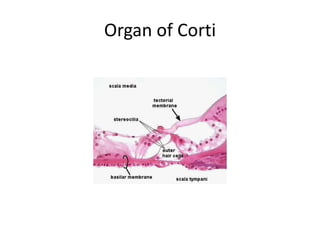
The document provides an eye and ear study guide that summarizes key structures and features. For the eye, it describes the three tunics (layers) that make up the eye wall, as well as internal structures like the aqueous and vitreous compartments, lens, zonular fibers, and retina. It also summarizes key features of the eyelid. For the ear, it outlines the external structures of the auricle and external auditory meatus, as well as the middle ear ossicles and auditory tube, and mentions the two main components of the inner ear.