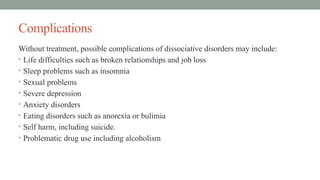
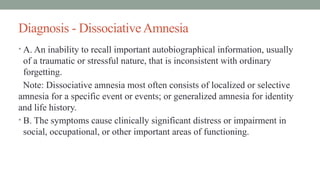
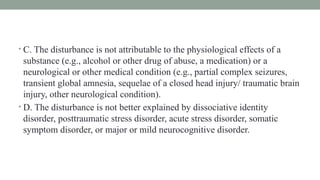
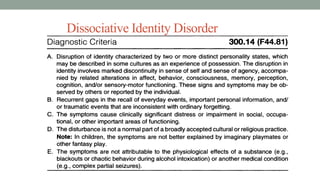
Dissociative disorders involve episodes of disconnection from the self or environment, significantly impacting daily life. These include dissociative amnesia, dissociative fugue, depersonalization disorder, and dissociative identity disorder, often linked to childhood trauma or stressful events, and can lead to various complications if untreated. Treatment ranges from psychotherapy and medication to stress management strategies.