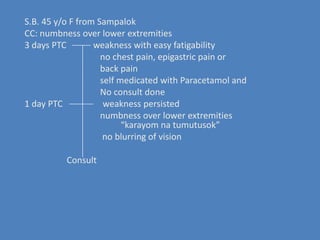
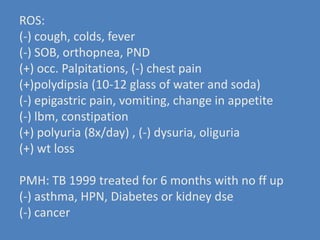
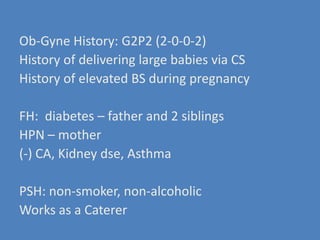
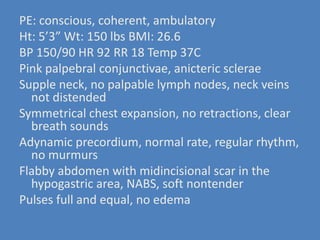
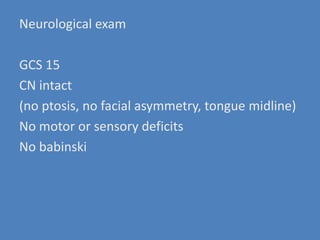
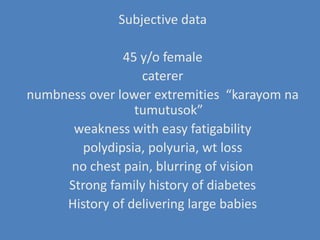
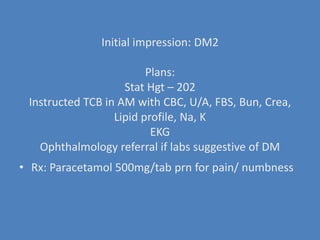
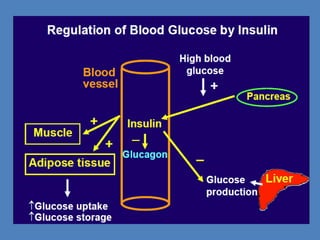
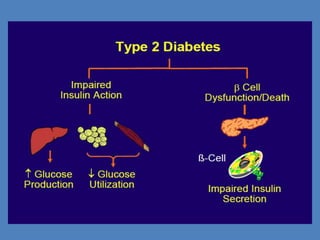
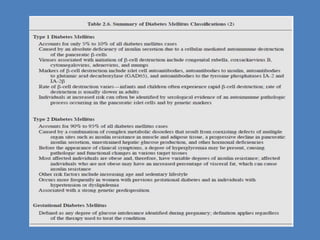
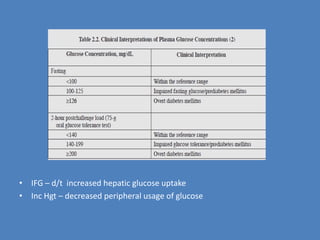
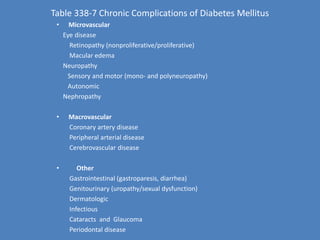
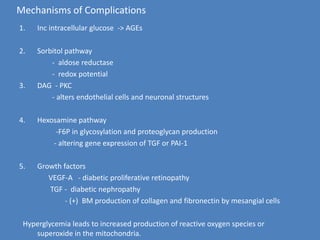
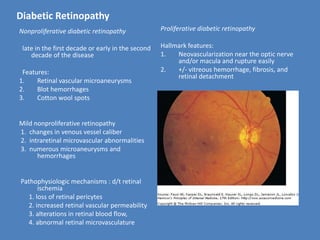
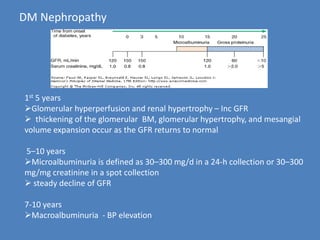
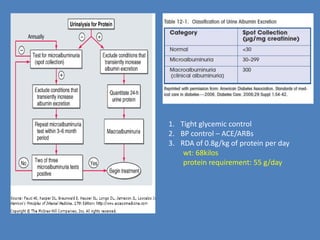
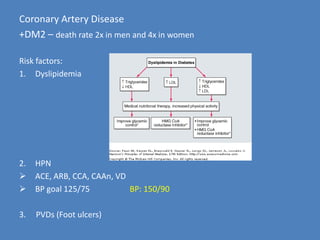
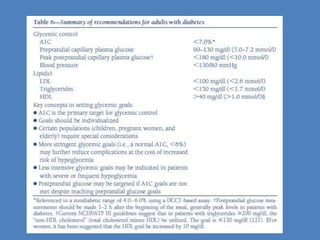
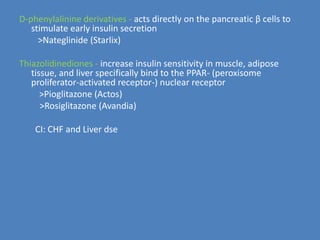
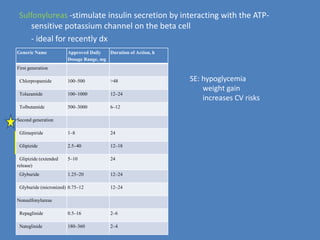
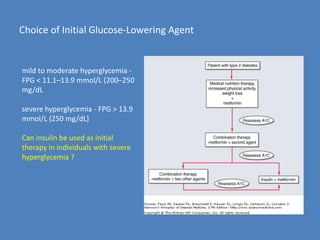
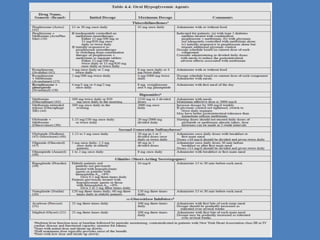
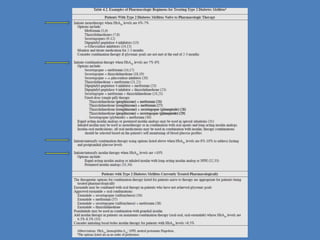
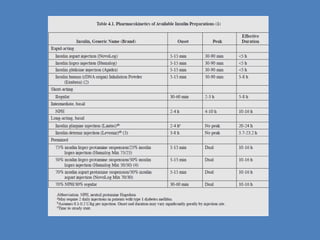
This document discusses diagnosing and managing diabetes. It presents the case of a 45-year-old female who presented with numbness and weakness in her lower extremities. Her initial impression was type 2 diabetes mellitus based on her family history, symptoms of polydipsia and polyuria, and weight loss. The document then reviews diabetic complications, treatment options, and guidelines for managing blood glucose, blood pressure, lipids, and other risk factors.