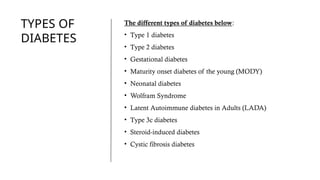
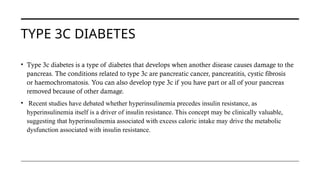
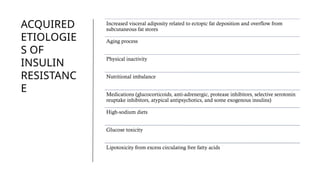
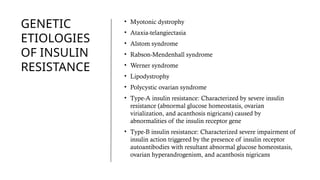
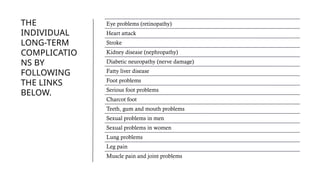
This comprehensive presentation explores Diabetes Mellitus, a chronic metabolic disorder that affects millions worldwide. It covers the different types of diabetes (Type 1, Type 2, Gestational, Type 3c, MODY, and more), underlying causes like insulin resistance, genetic and acquired etiologies, and long-term complications.
Key slides focus on:
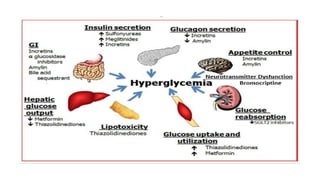
• Pathophysiology of insulin resistance
• Pancreatic β-cell dysfunction in T2D
• Risk factors like obesity, diet, ethnicity, and medications
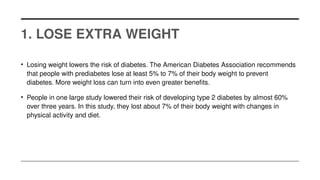
• Prevention strategies including lifestyle modifications and healthy eating
Ideal for students, public health professionals, and anyone seeking a detailed yet understandable overview of diabetes and how to manage or prevent it.