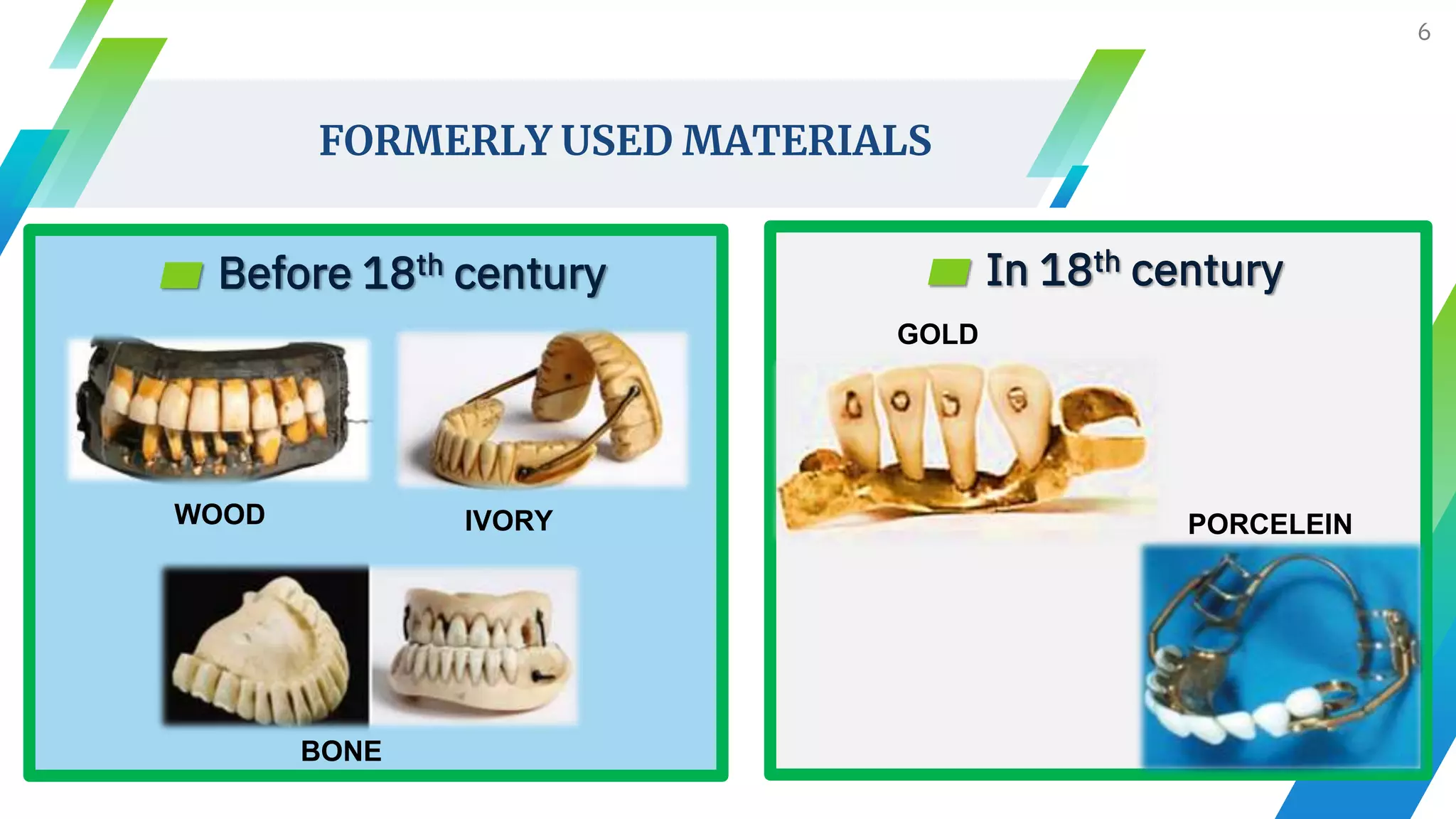
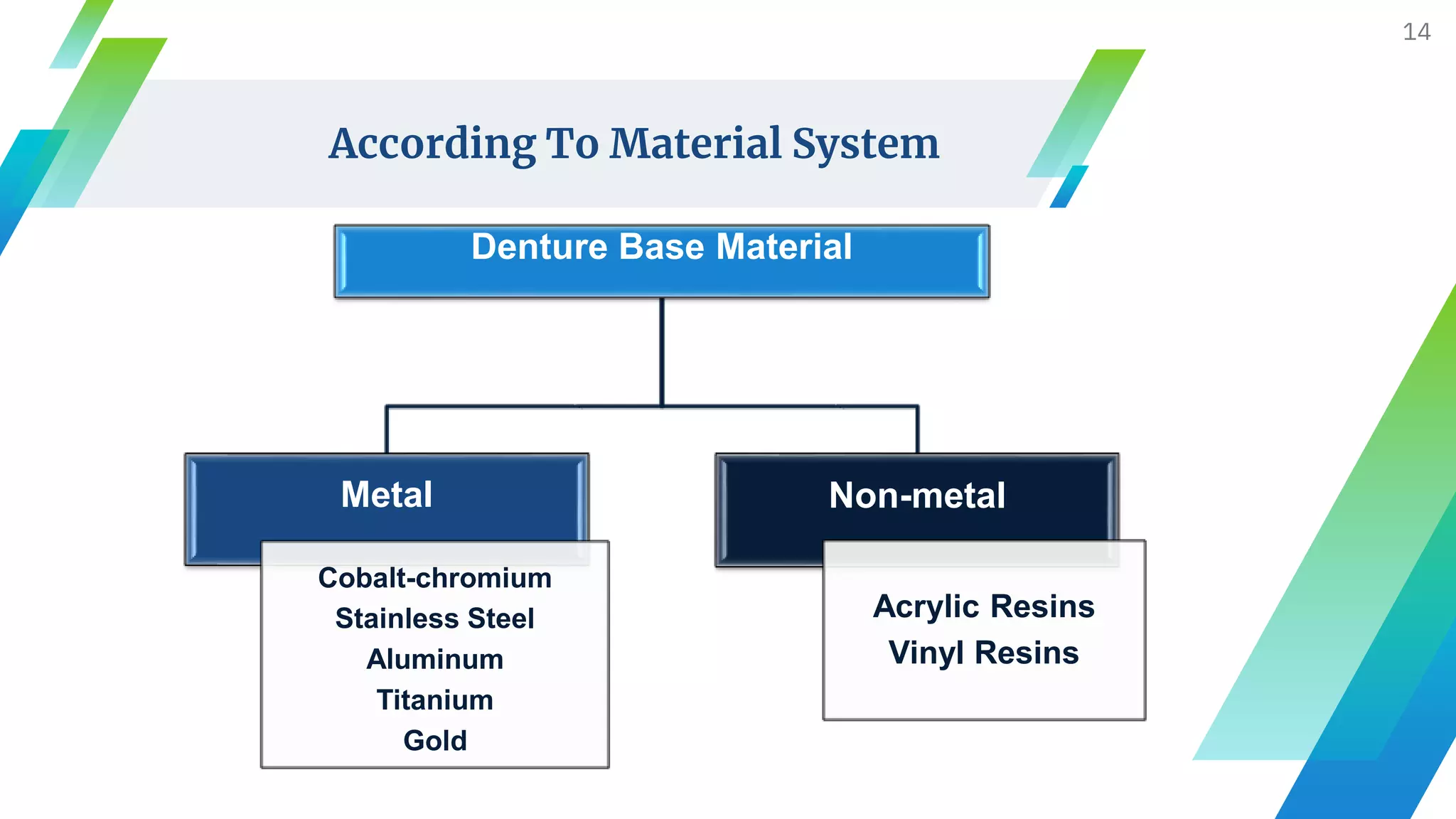
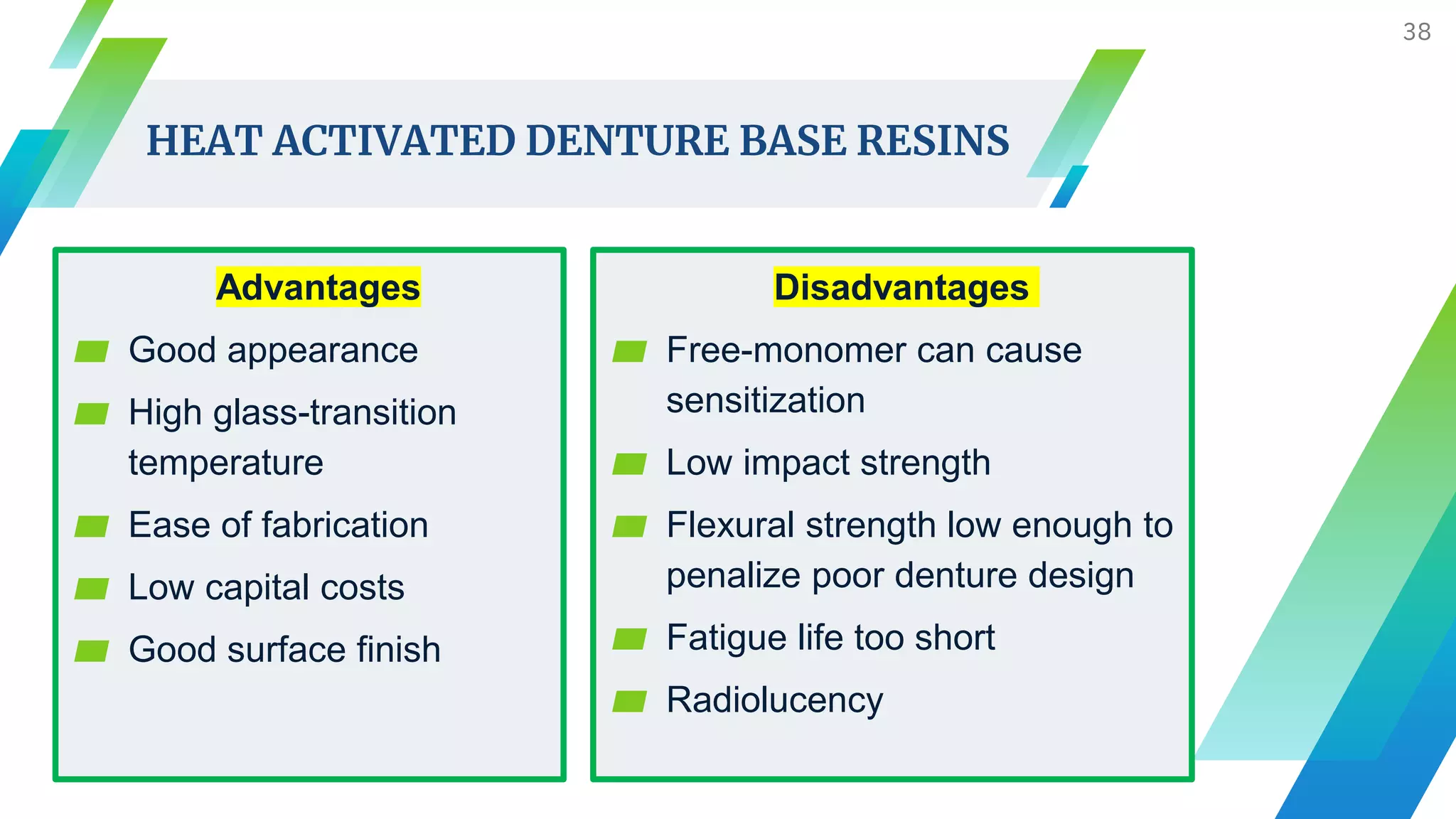
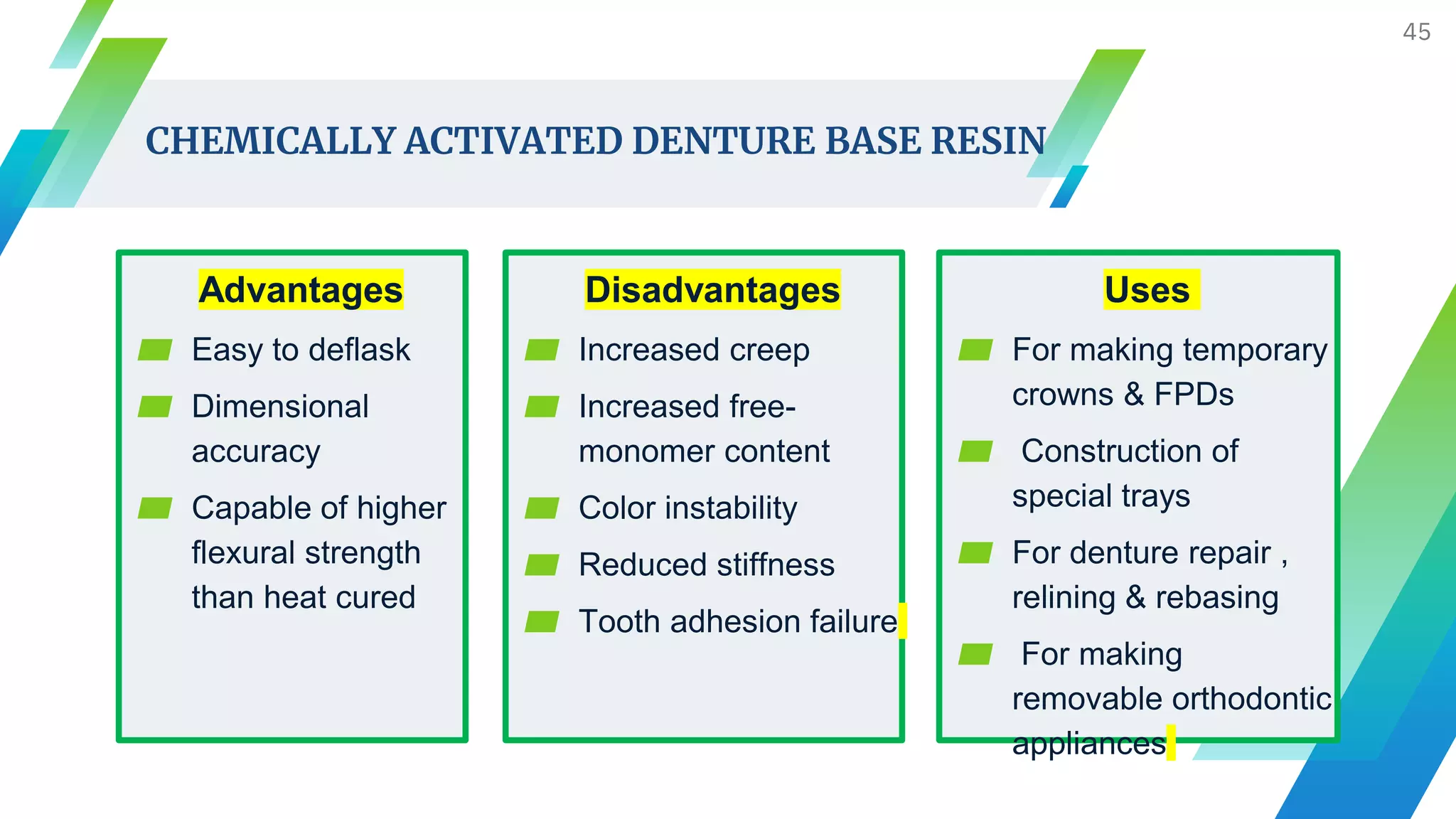
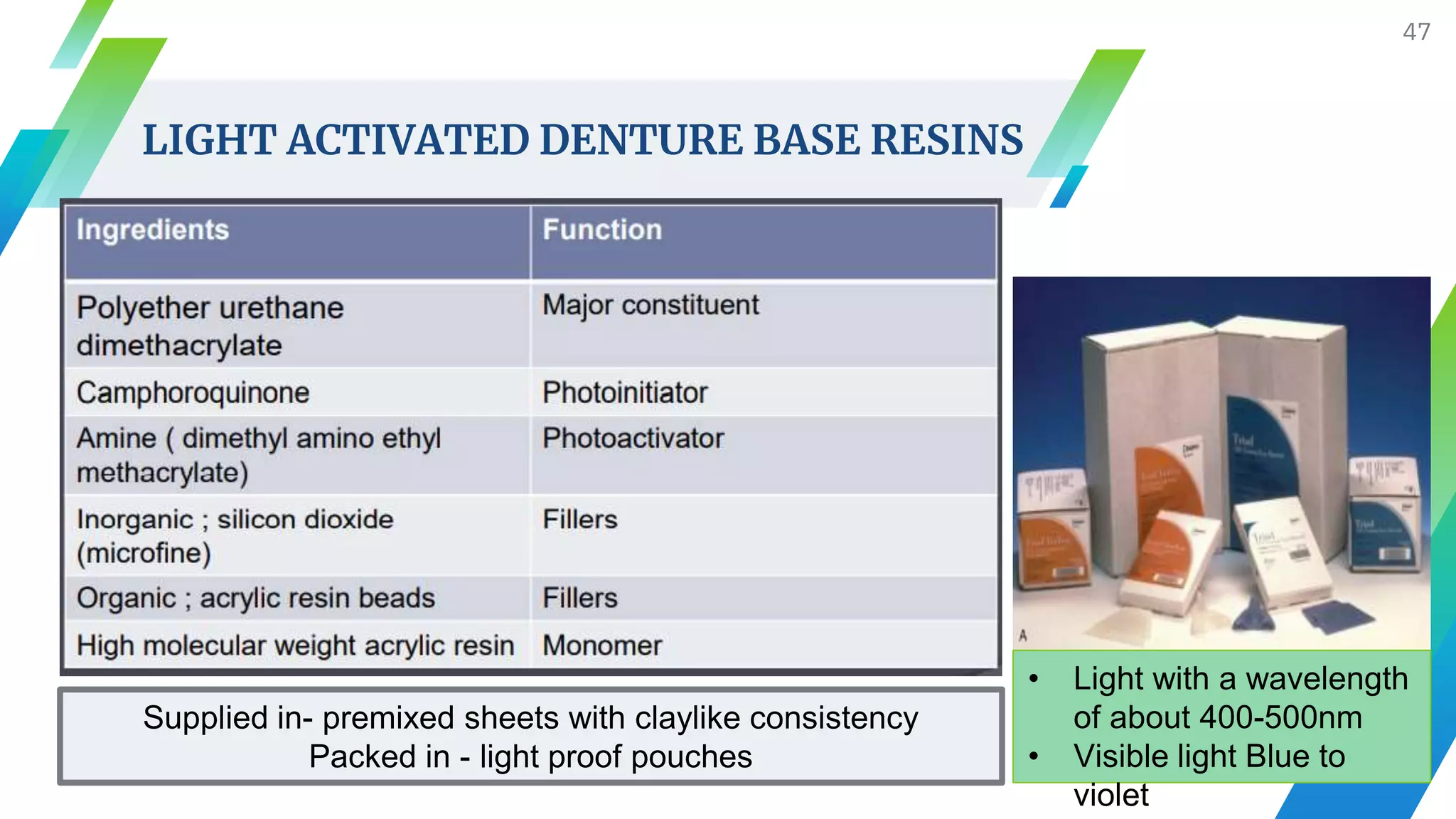
The document discusses various materials used for denture bases, including historical progression from organic materials to modern polymers and metals. It outlines the ideal properties for denture base materials, classifications of denture bases, and recent advancements in materials such as hypoallergenic resins and thermoplastics. Key advantages and disadvantages of metal versus resin bases, as well as polymerization methods, are also highlighted.