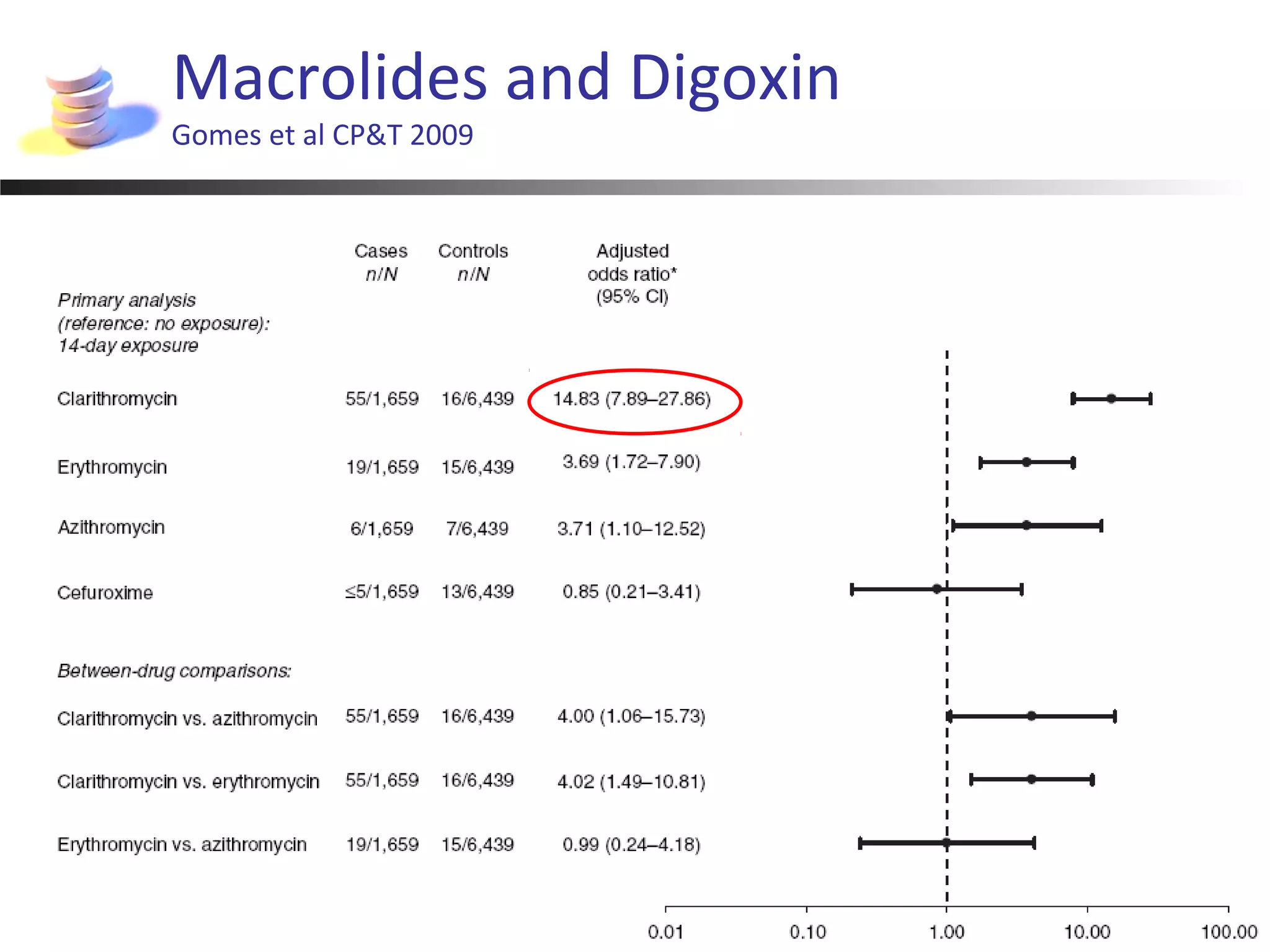
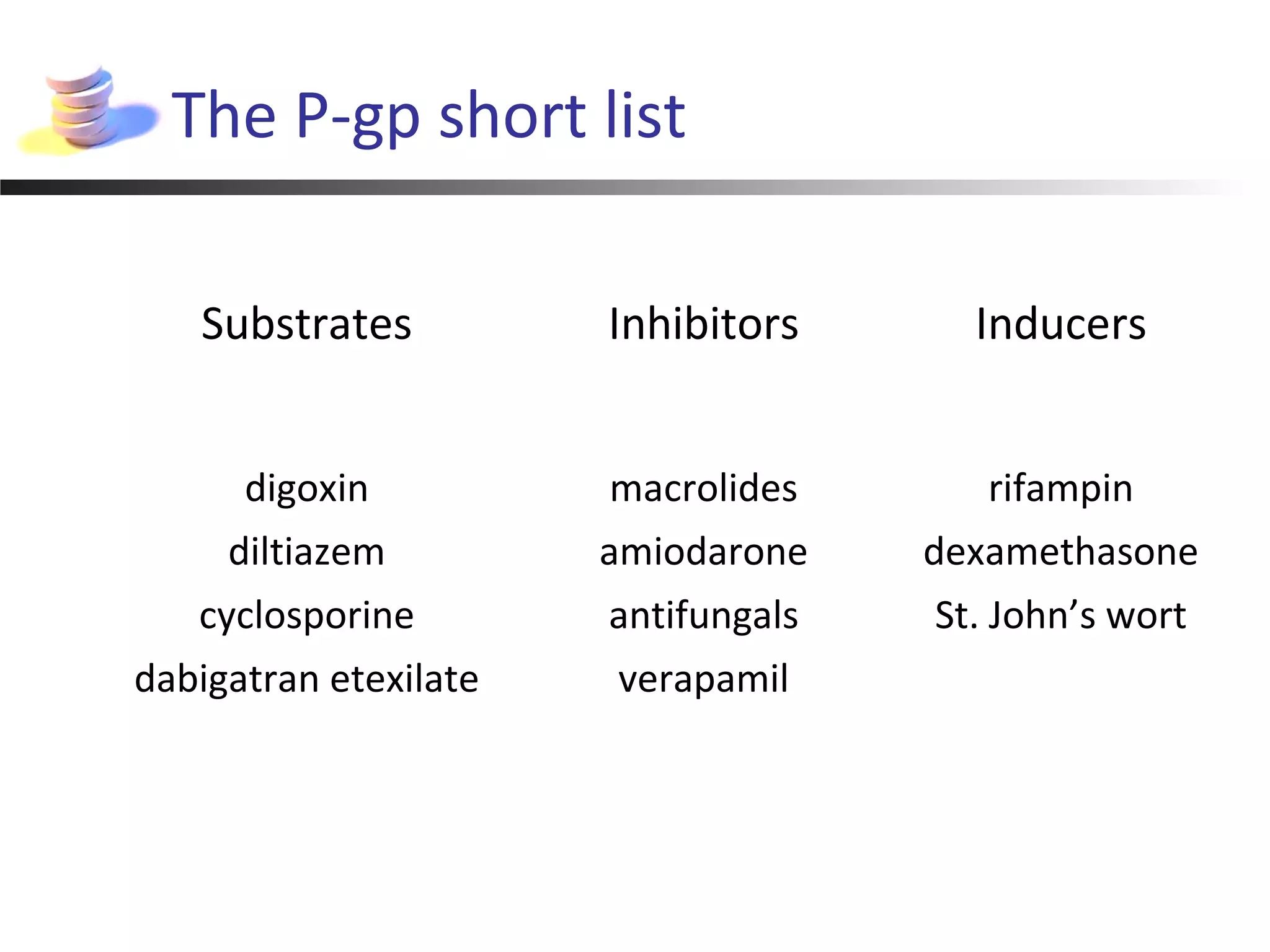
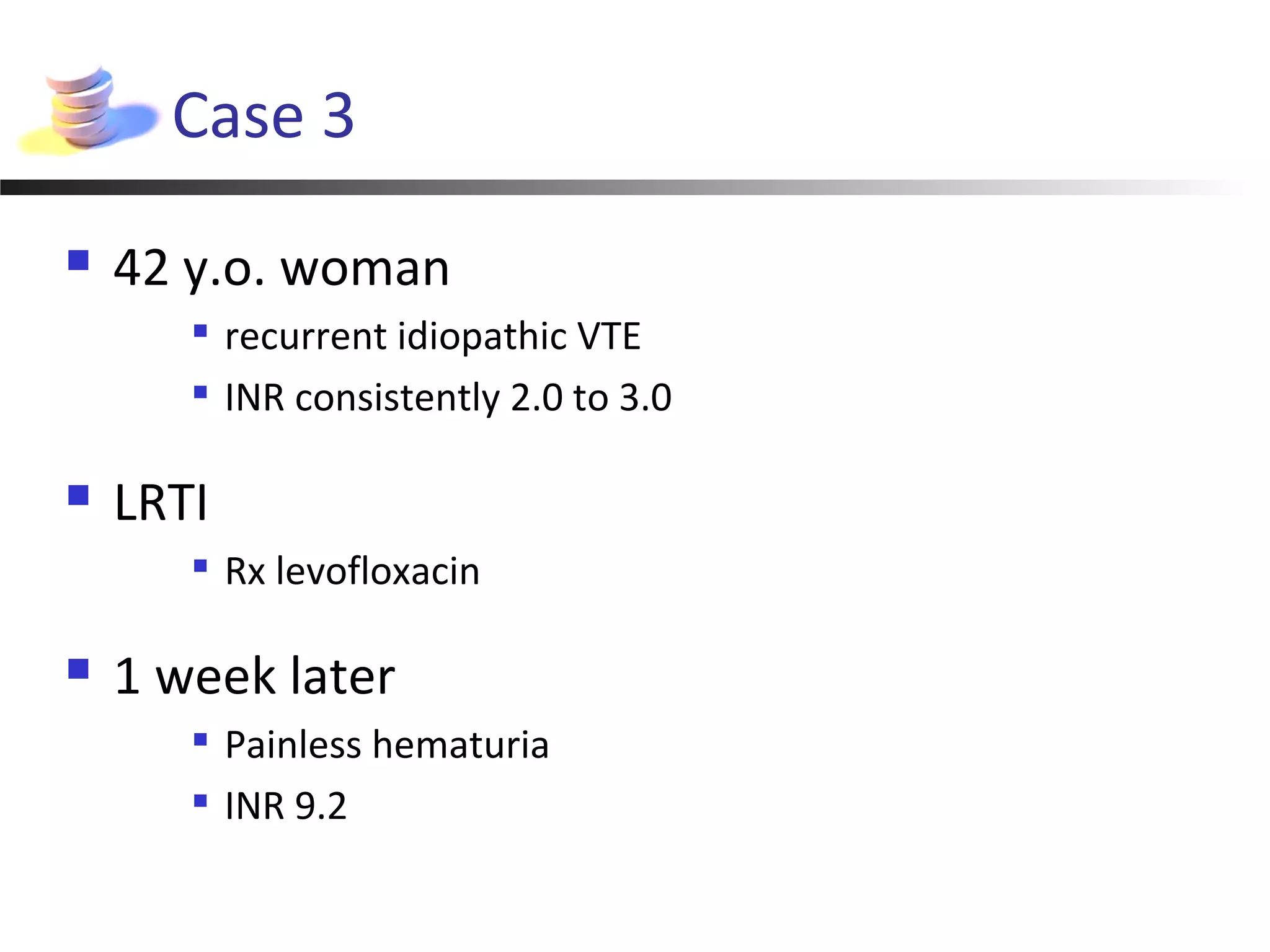
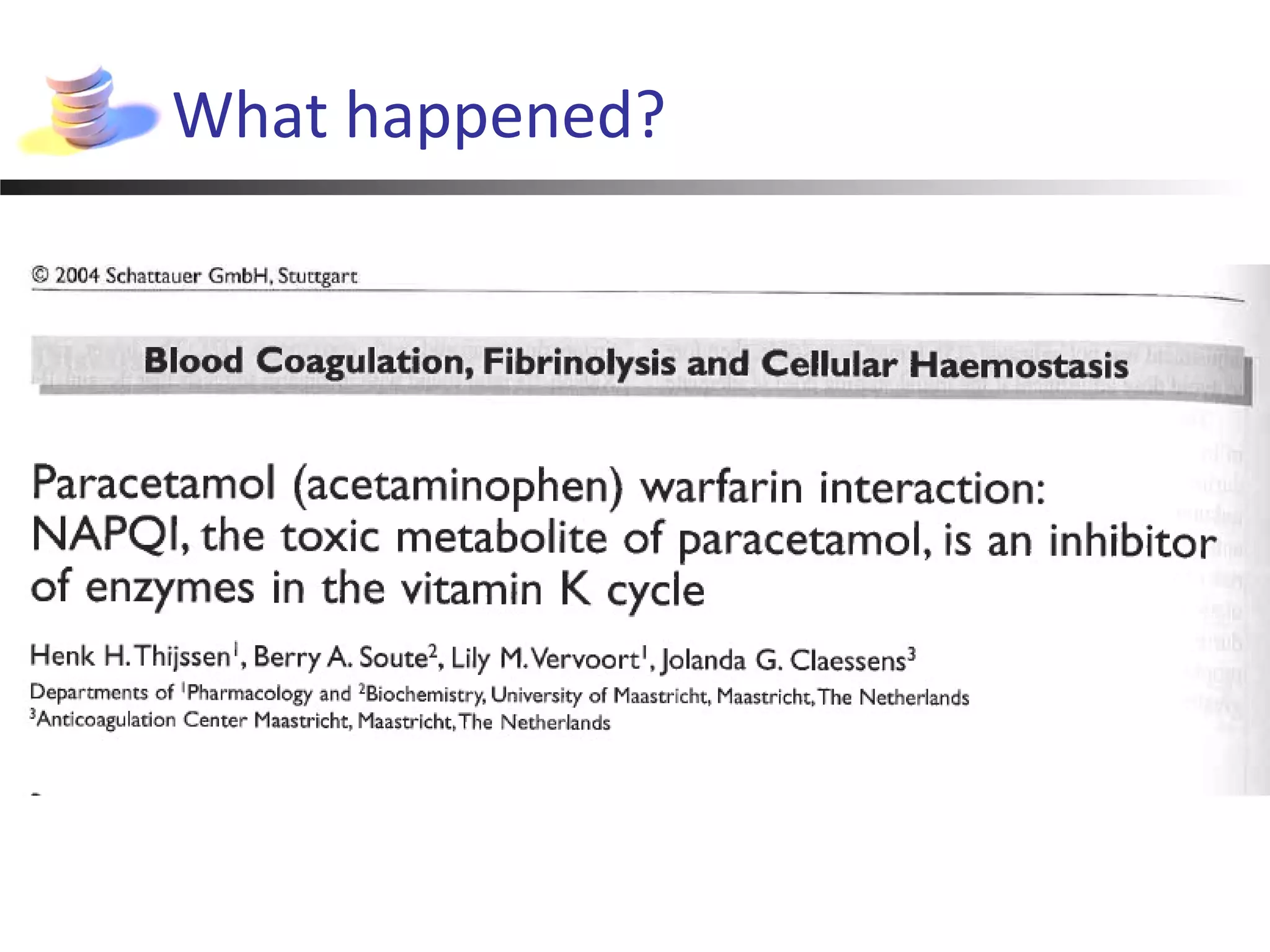
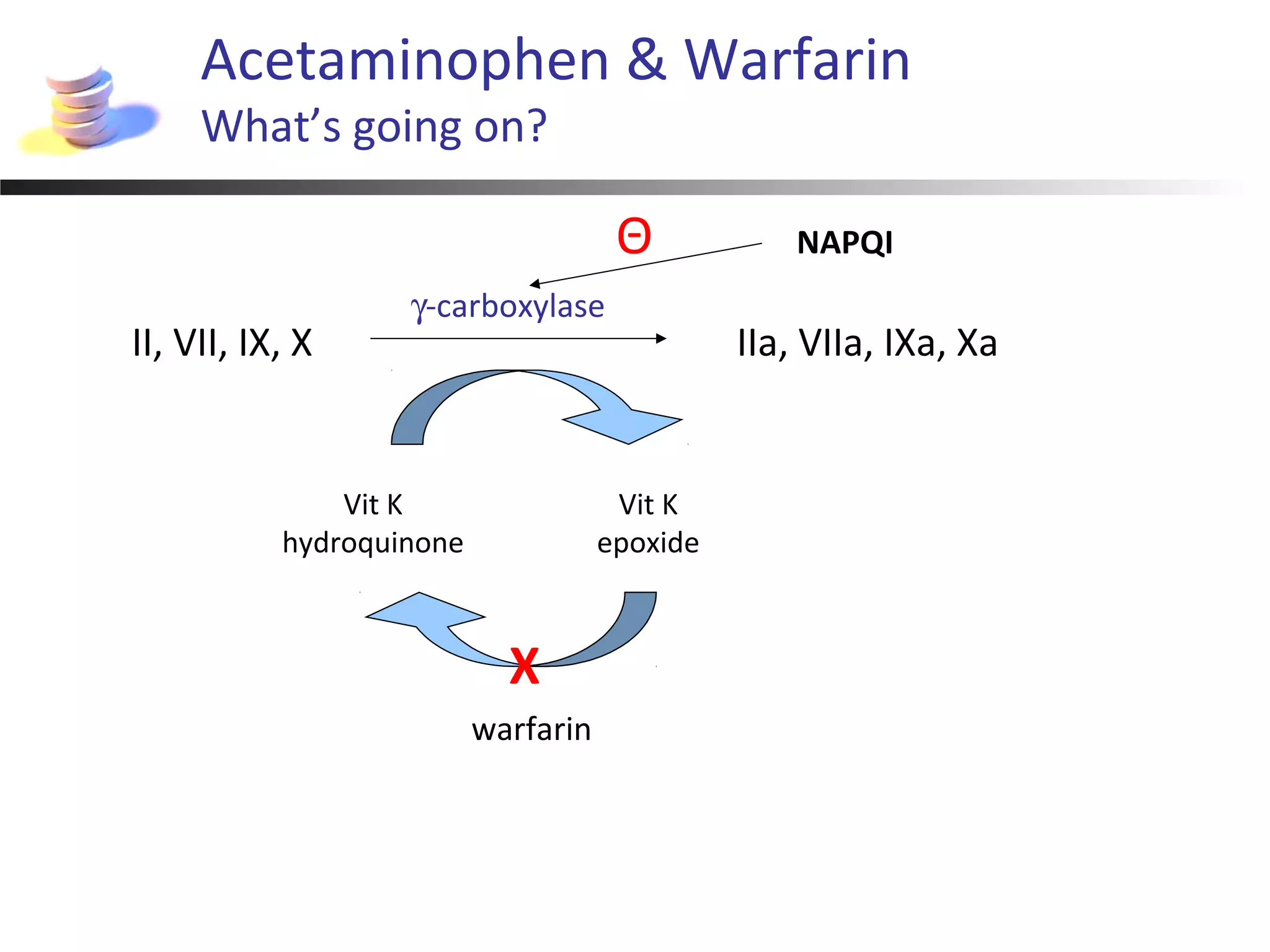
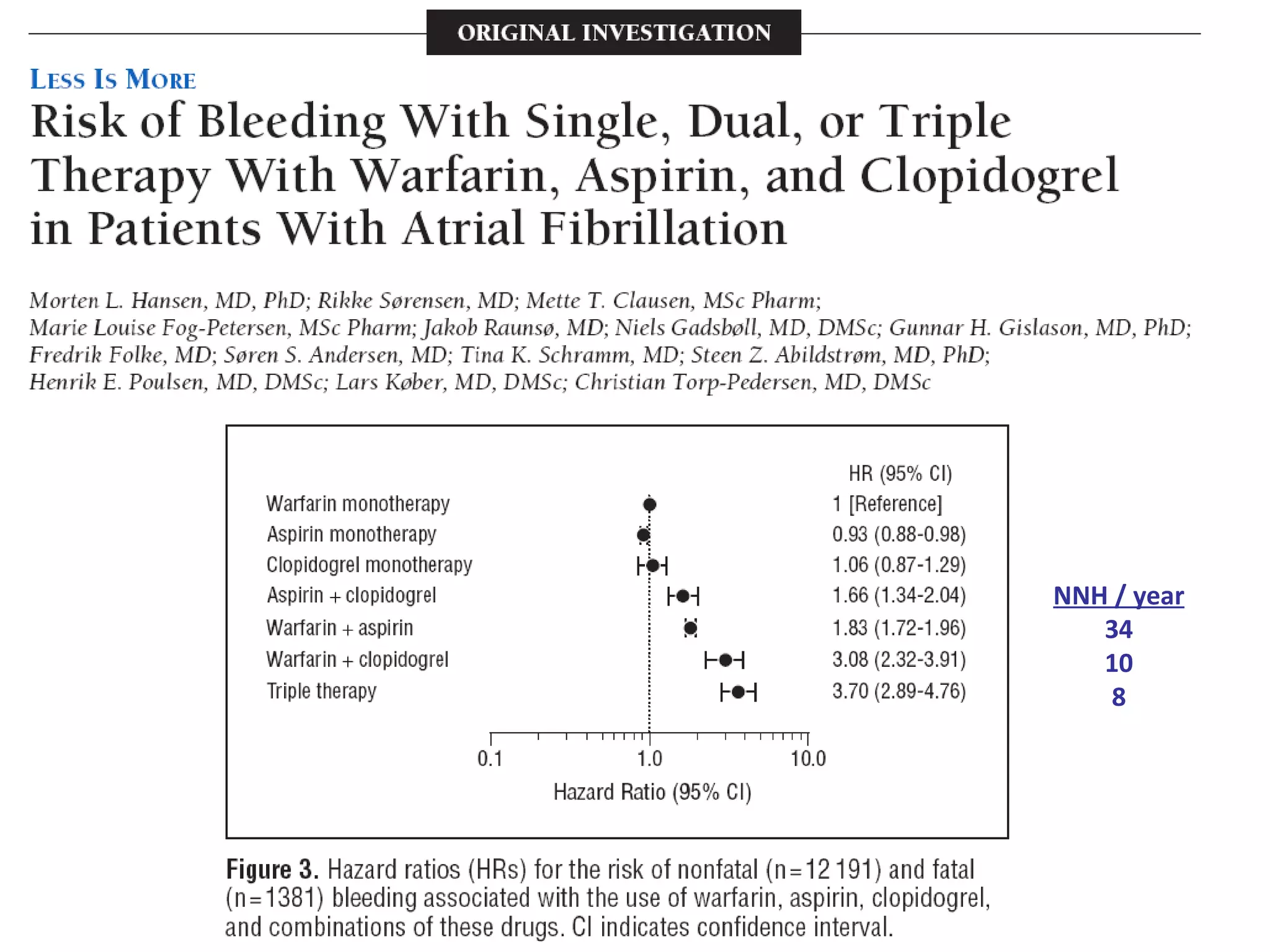
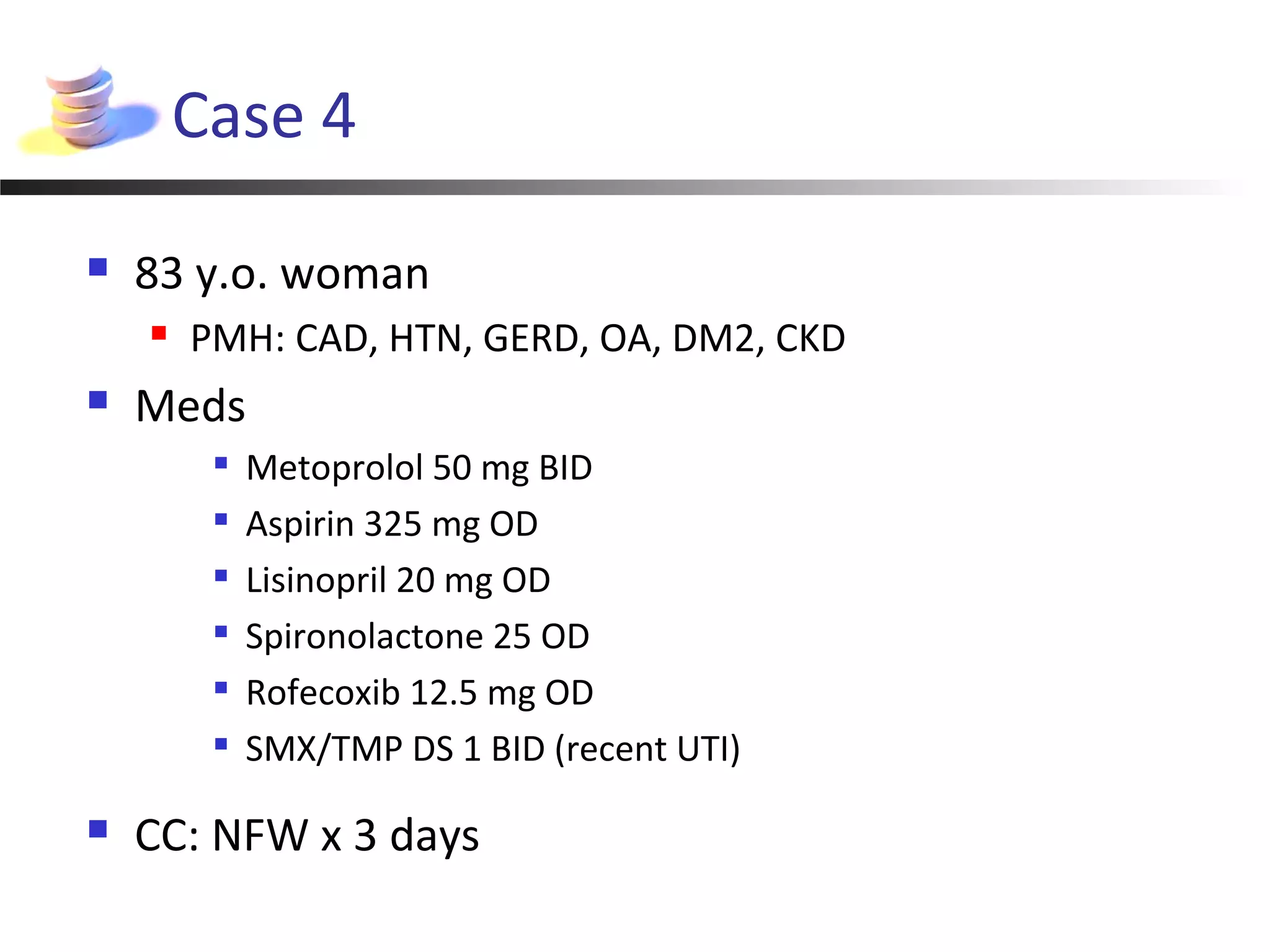
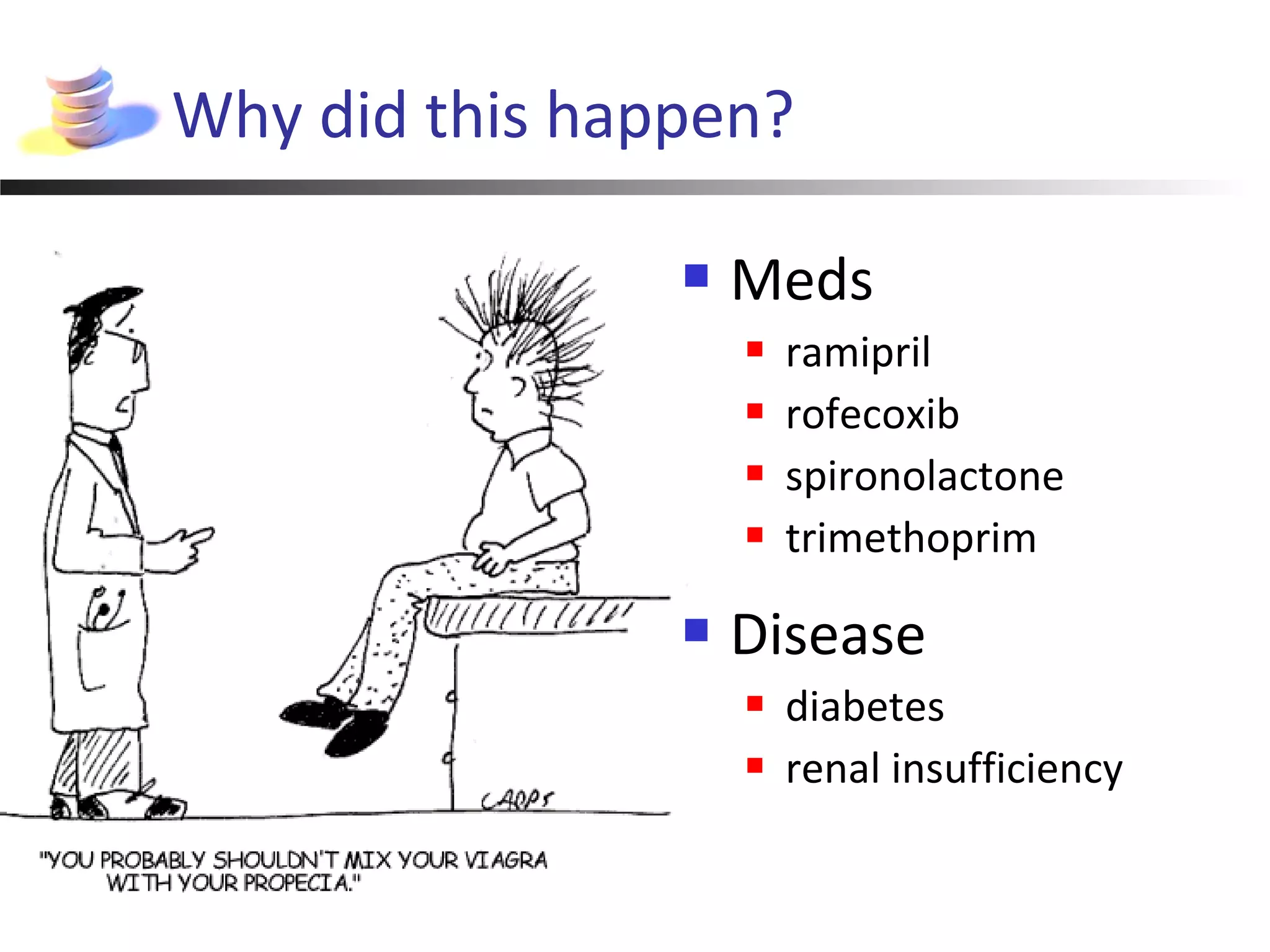
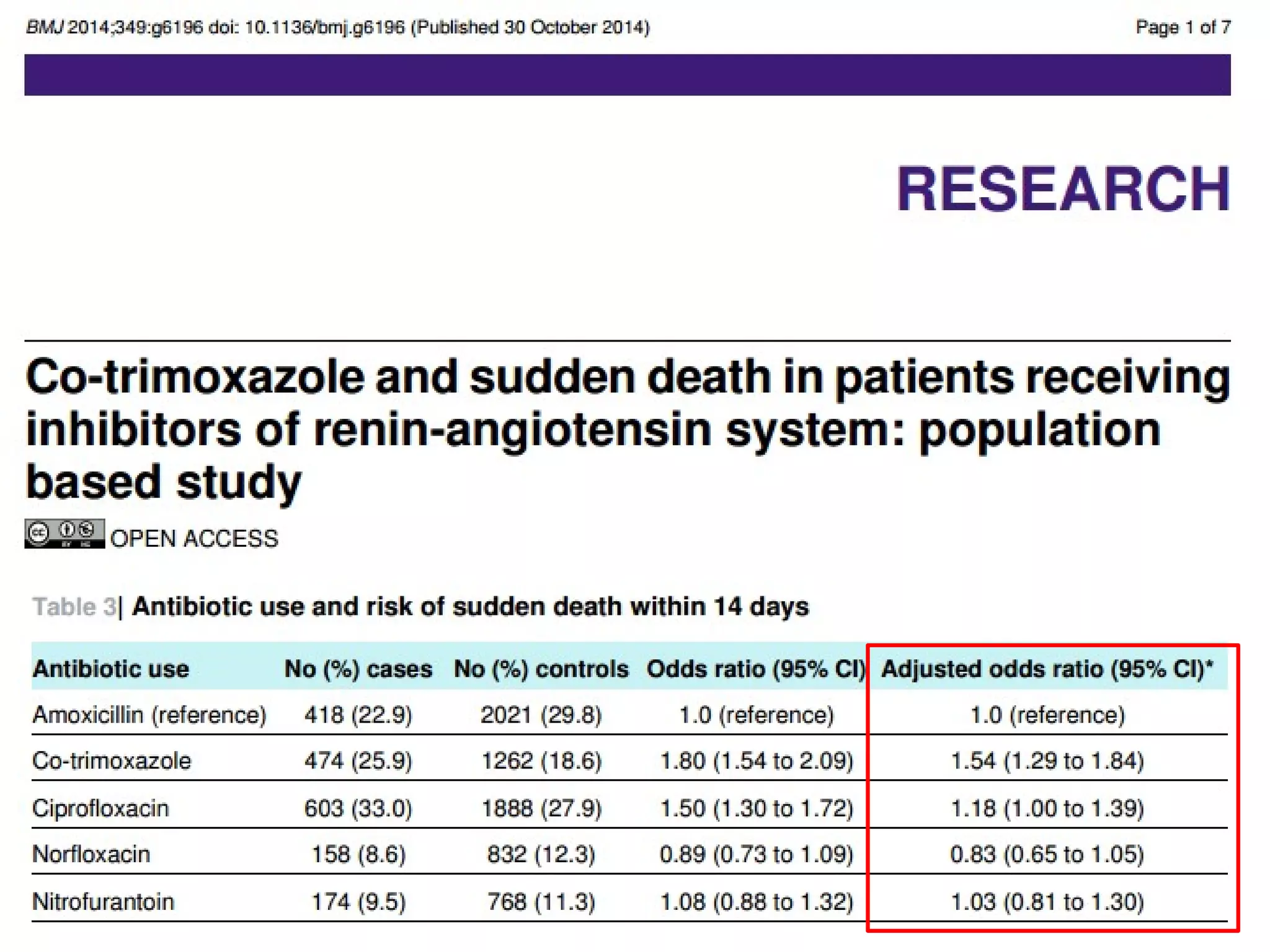
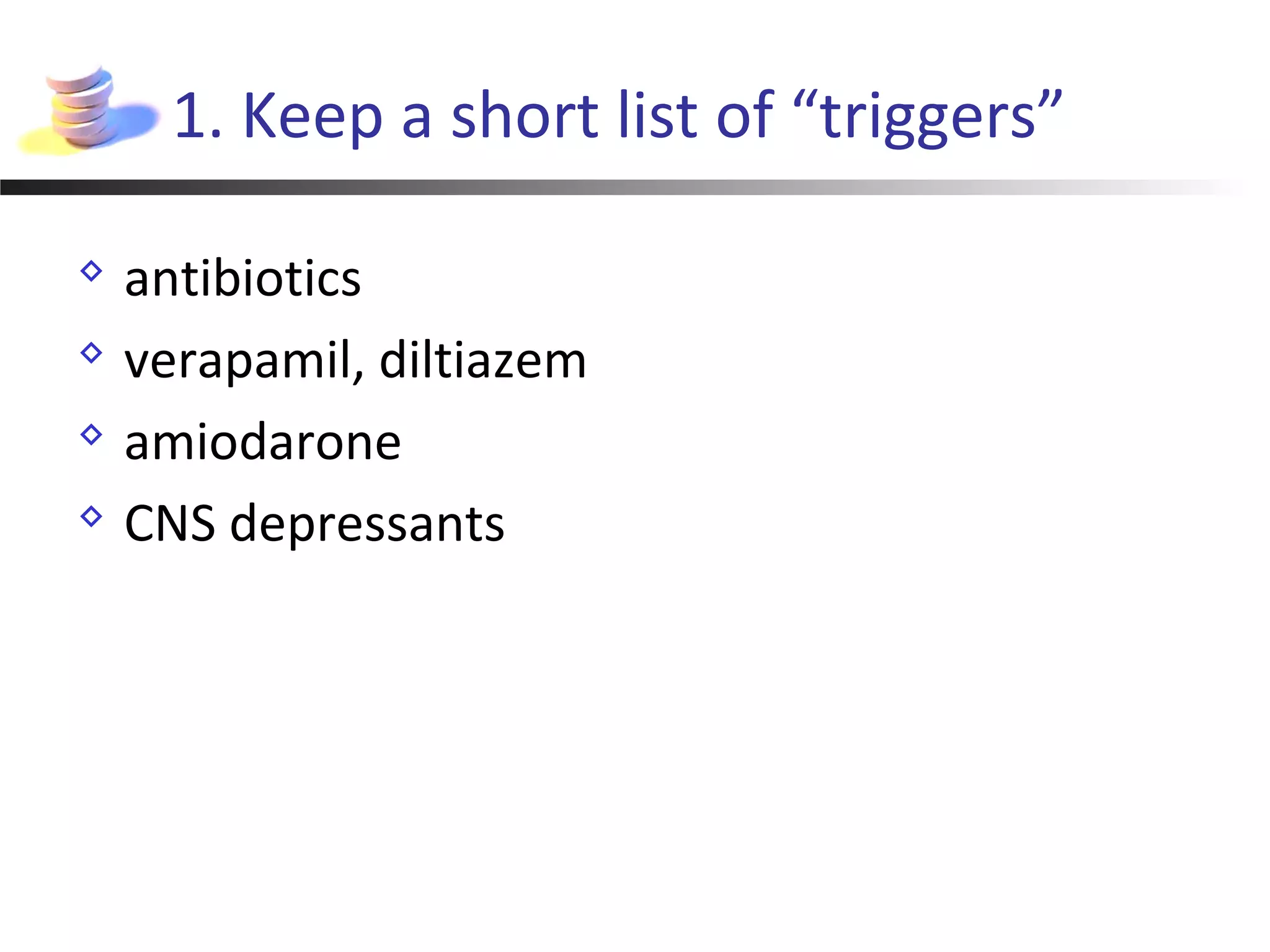
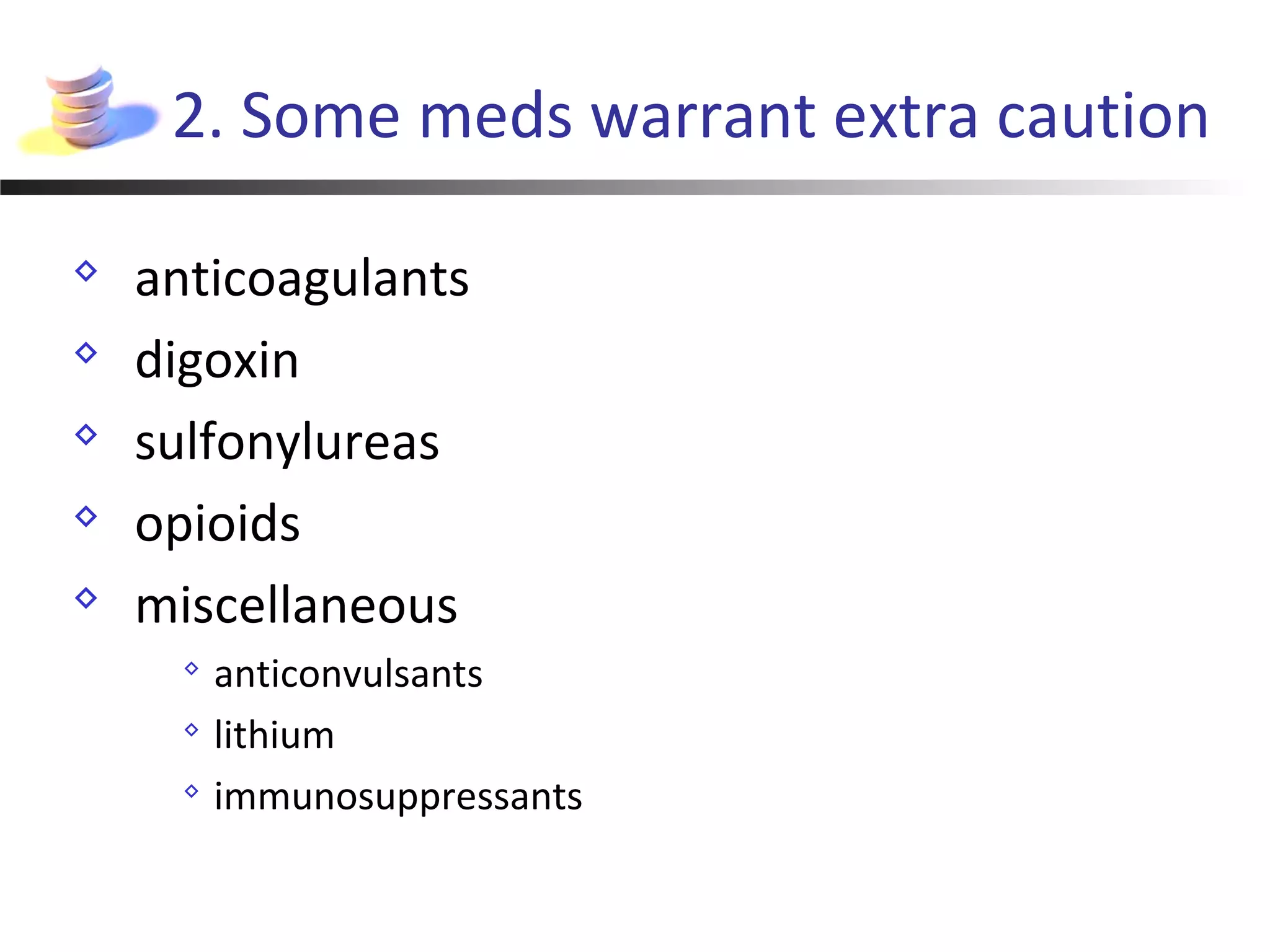
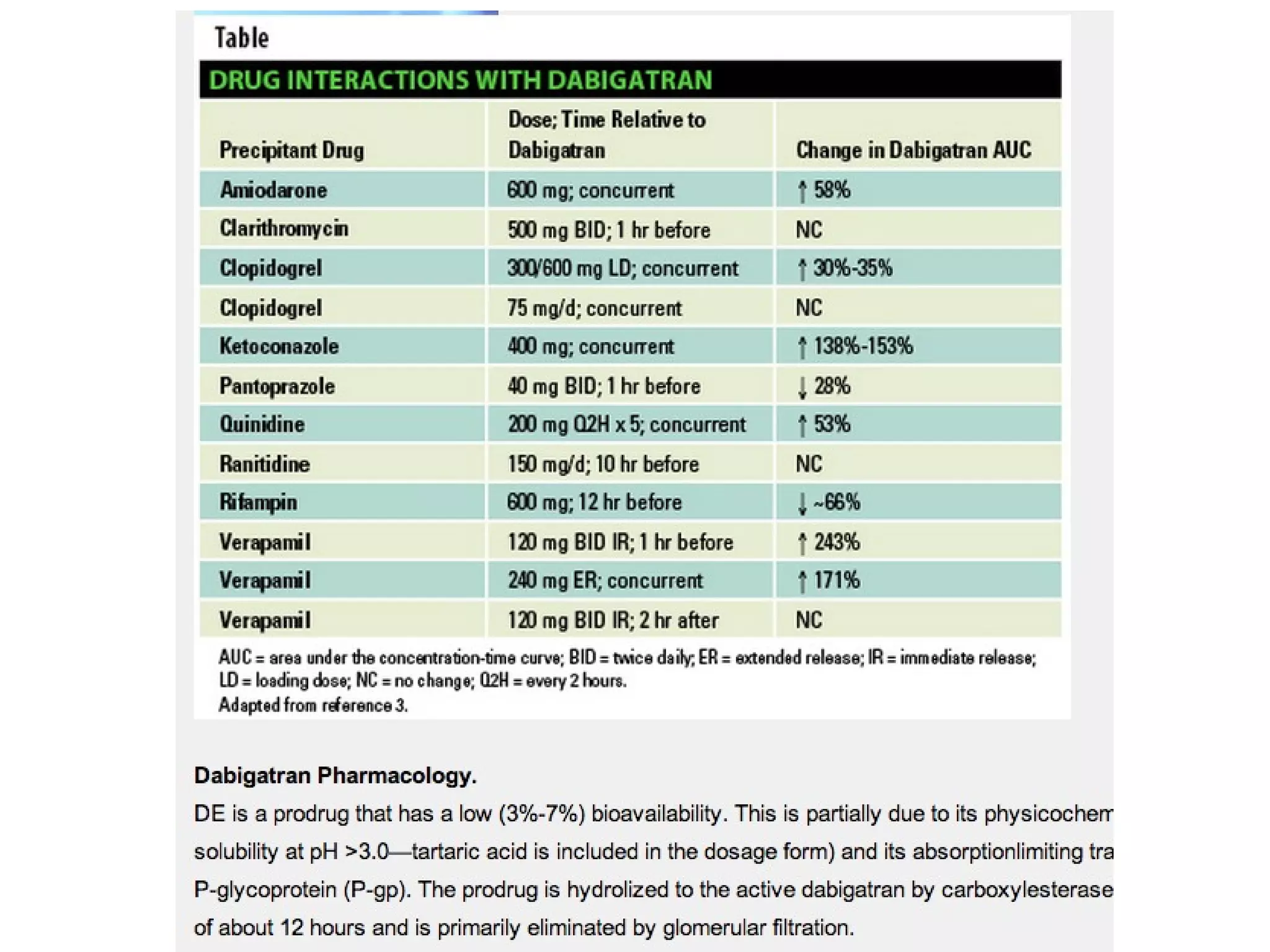
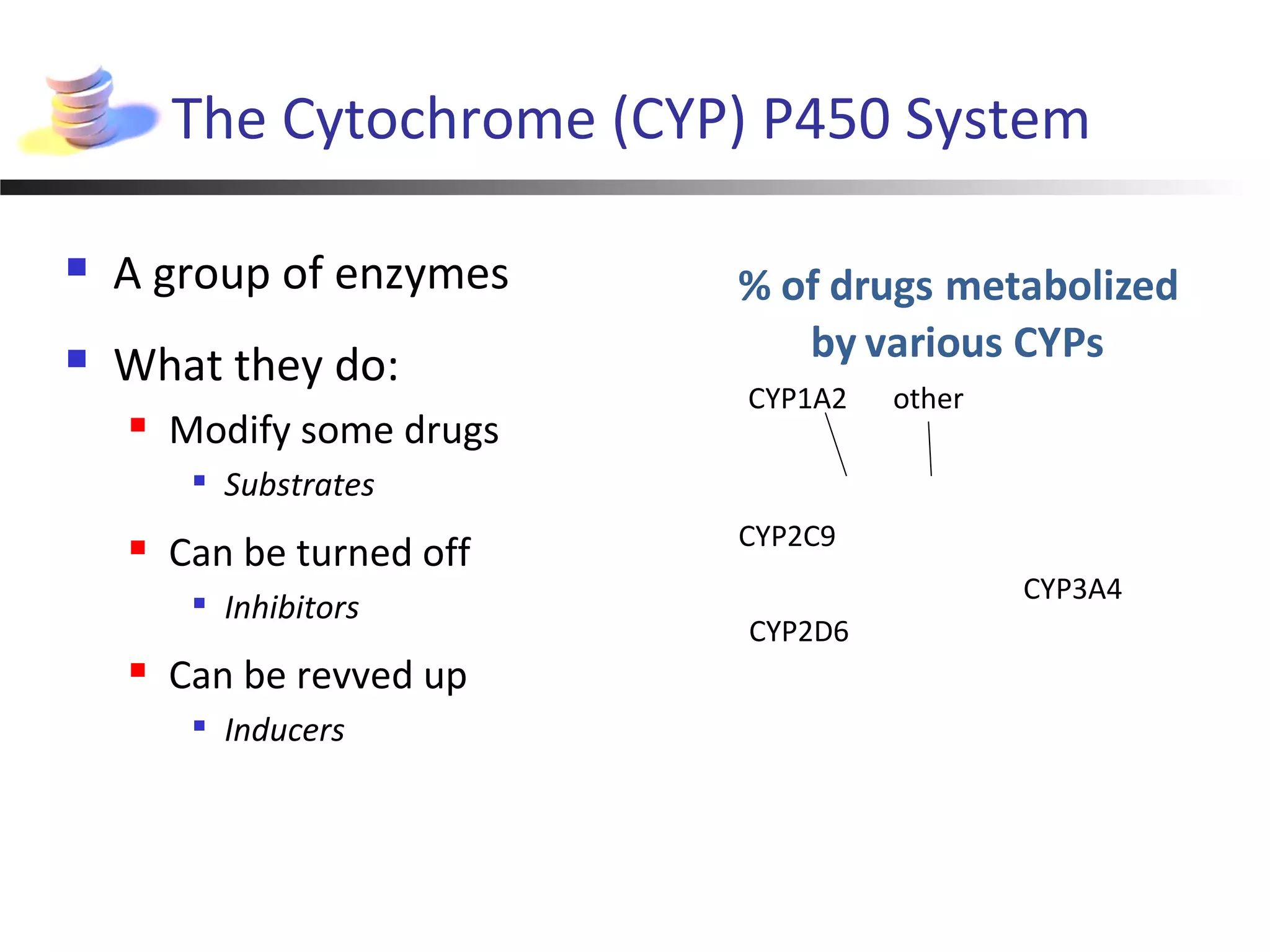
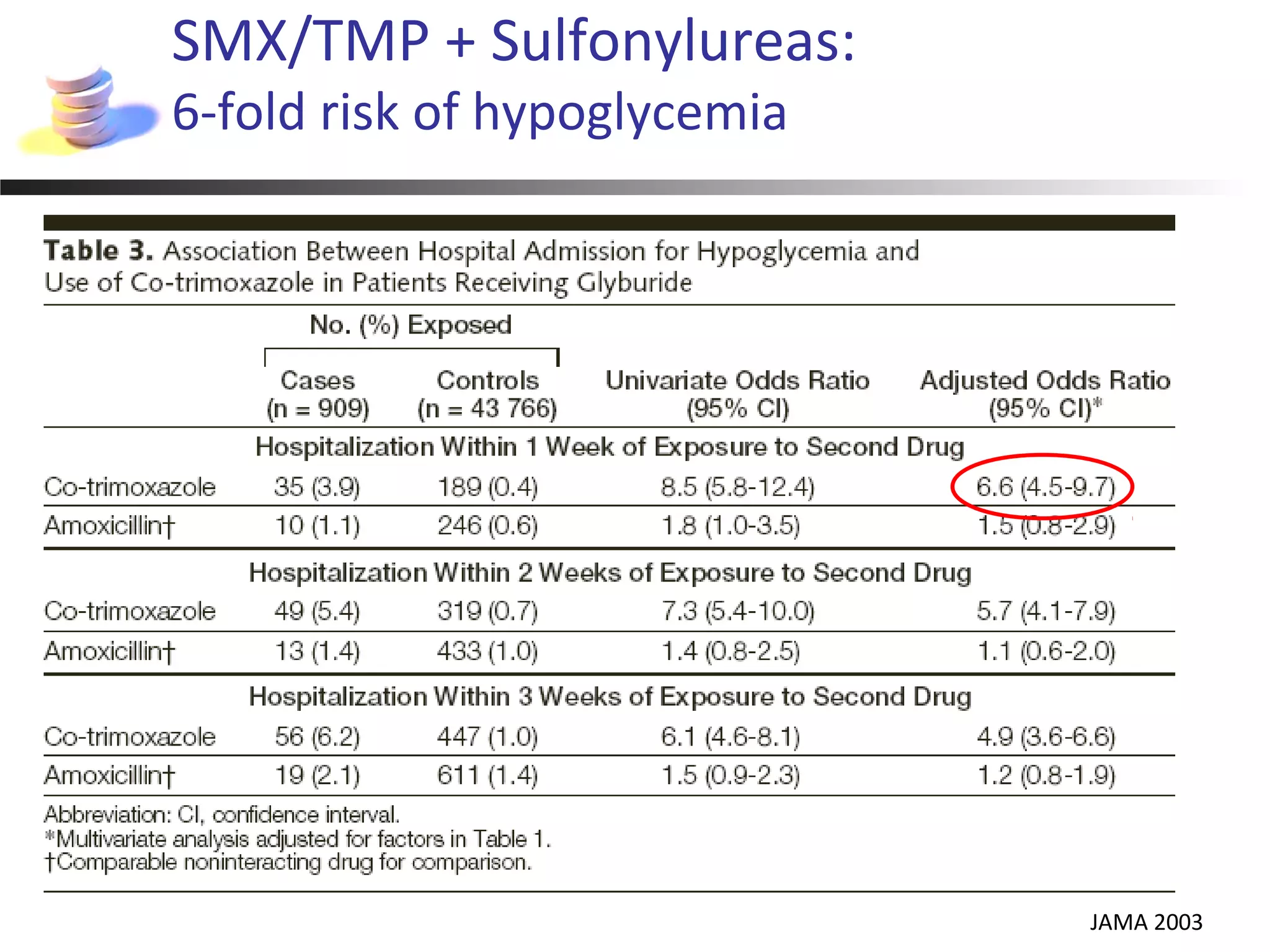
The document discusses lethal drug-drug interactions (DDIs) and how to avoid them, emphasizing both pharmacokinetic and pharmacodynamic types. It presents several case studies illustrating the dangers of specific combinations, particularly involving common medications and the cytochrome P450 system. To mitigate risk, the document recommends maintaining awareness of high-risk drug combinations and suggests consulting pharmacists for safer alternatives.
![Frontmatter
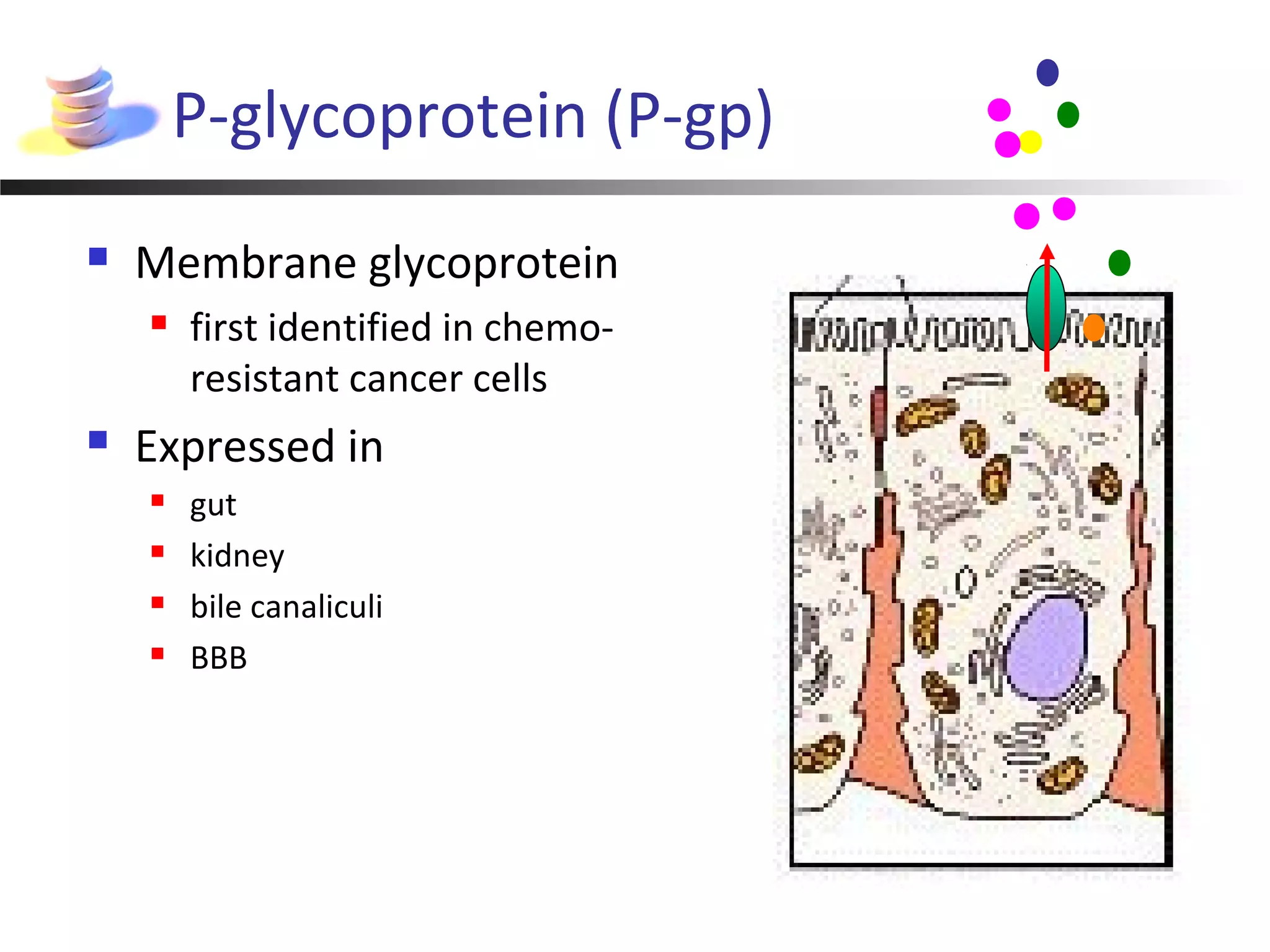
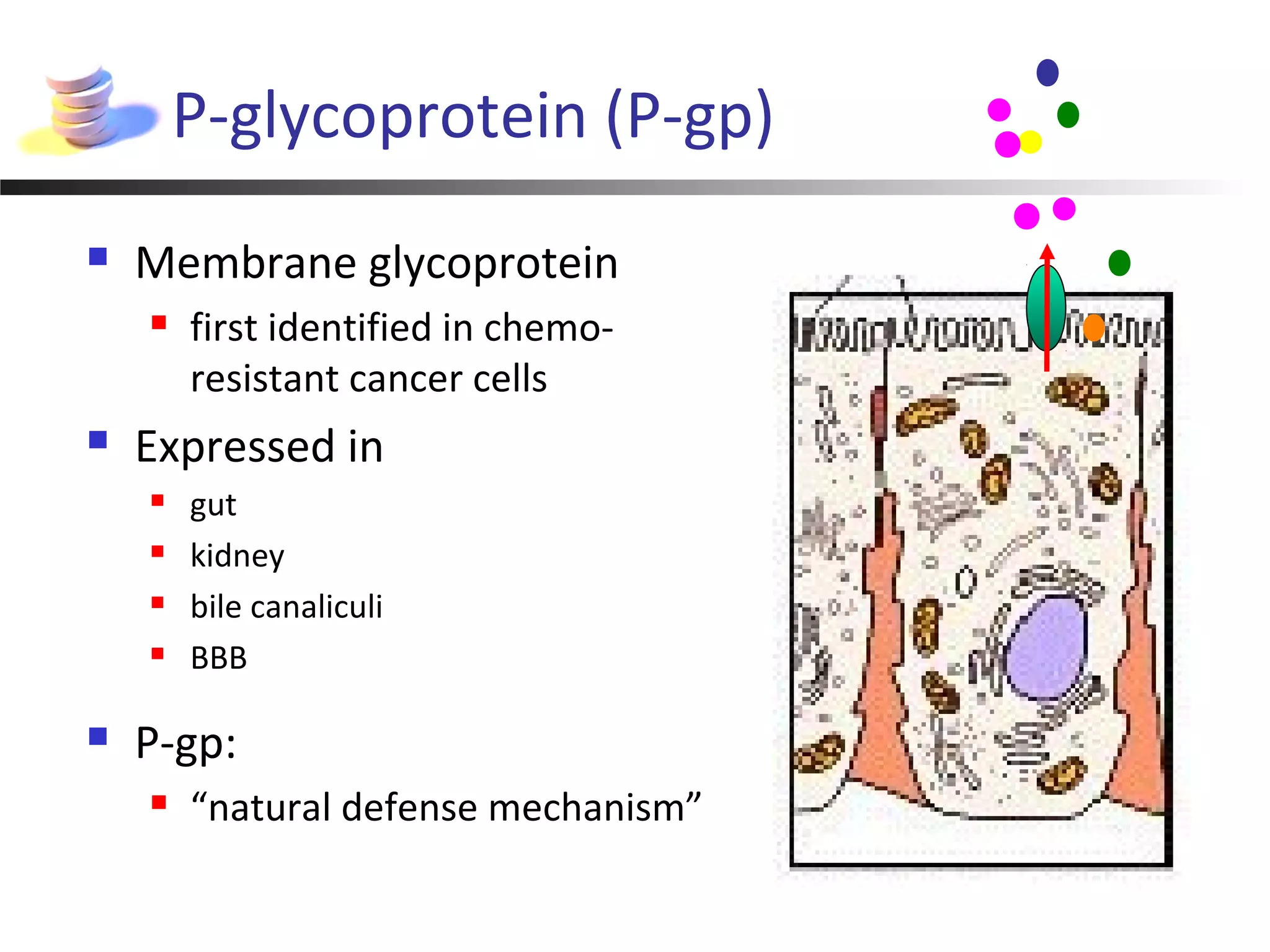
Drug-drug interaction (DDI):
Effect of one drug altered by use of another
Two types
Pharmacokinetic
One drug alters the level of another time ->
Drug B
[DrugA]](https://image.slidesharecdn.com/1050djuurlink-160523235953/75/David-Juurlink-Drug-Interactions-That-Can-Kill-and-How-to-Avoid-Them-2-2048.jpg)
![Frontmatter
Drug-drug interaction (DDI):
Effect of one drug altered by use of another
Two types
Pharmacokinetic
One drug alters the level of another
Pharmacodynamic
No change in drug levels
time ->
time ->[DrugA]
Drug B
Drug B
[DrugA]](https://image.slidesharecdn.com/1050djuurlink-160523235953/75/David-Juurlink-Drug-Interactions-That-Can-Kill-and-How-to-Avoid-Them-3-2048.jpg)
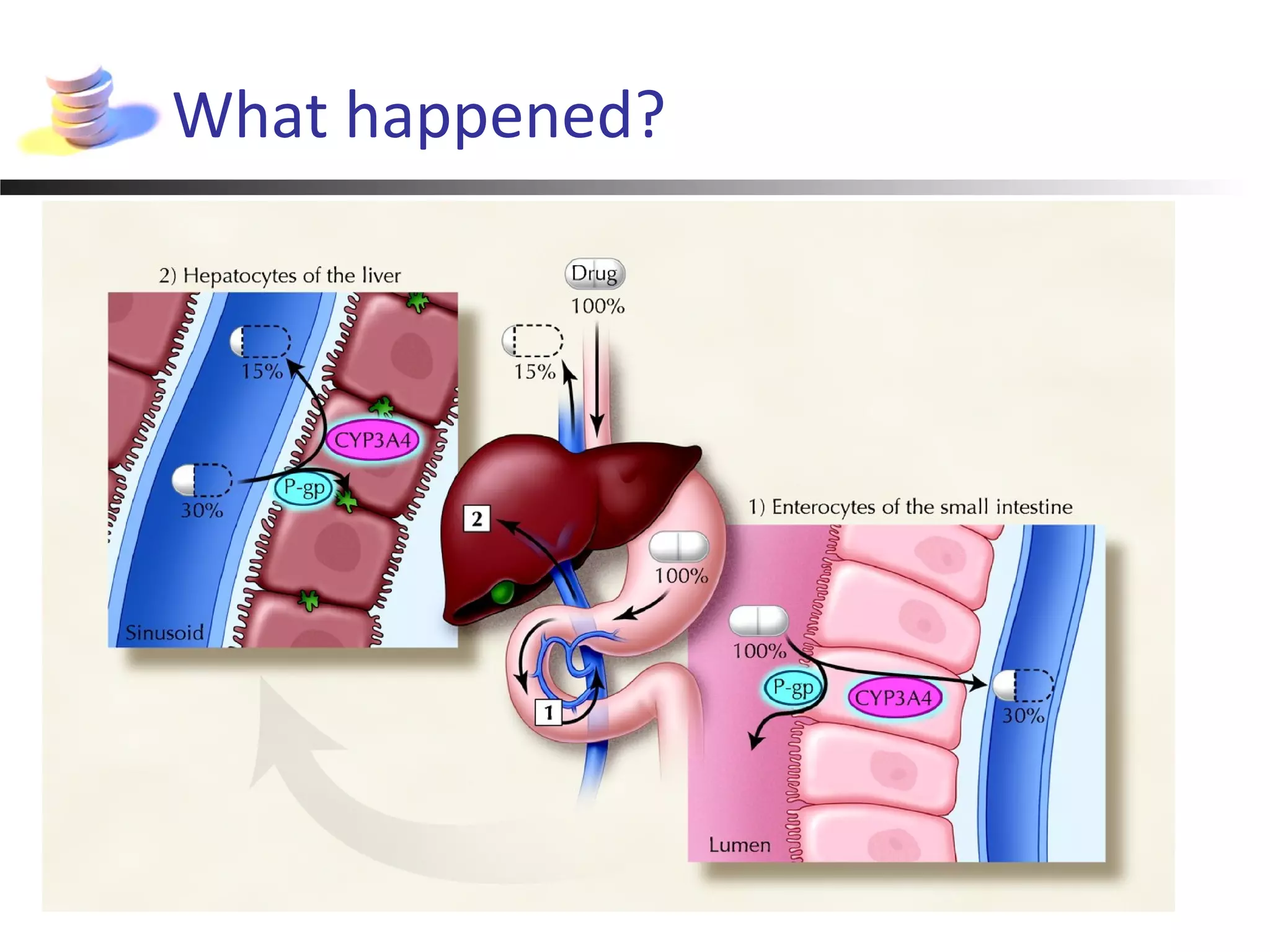
![[digoxin] 5.1 nmol/L (3.6 ng/mL)](https://image.slidesharecdn.com/1050djuurlink-160523235953/75/David-Juurlink-Drug-Interactions-That-Can-Kill-and-How-to-Avoid-Them-11-2048.jpg)