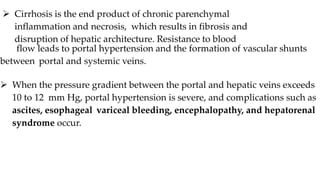
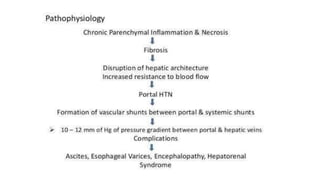
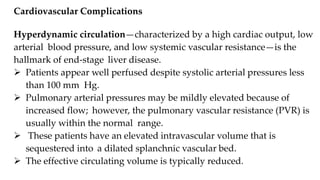
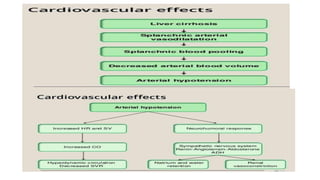
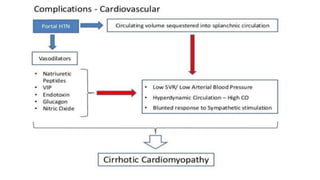
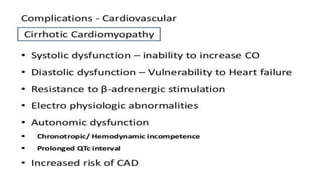
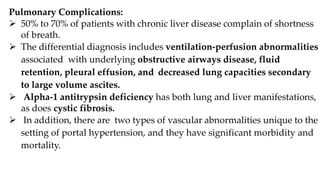
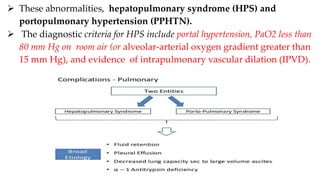
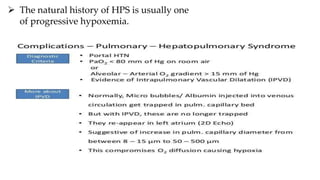
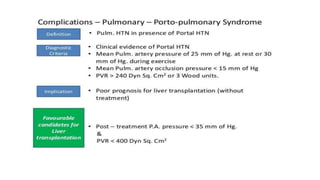
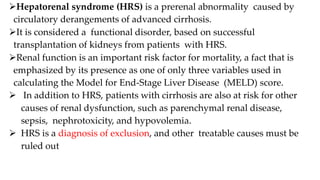
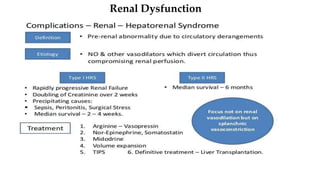
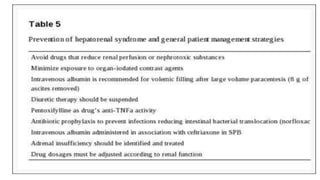
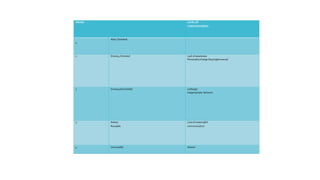
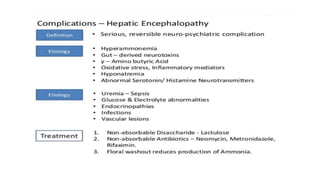
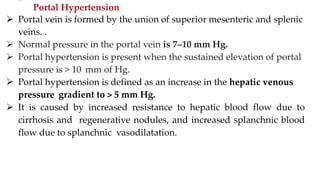
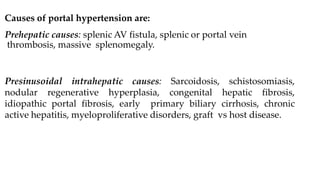
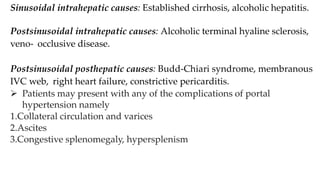
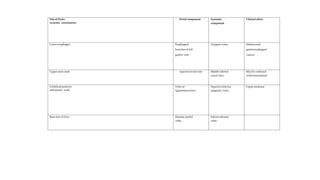
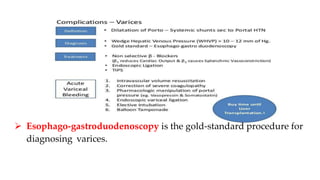
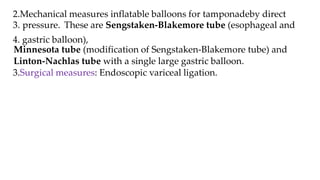
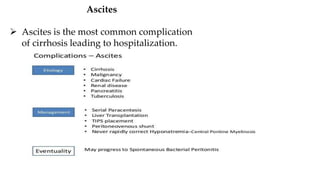
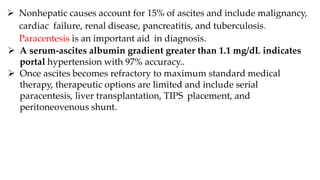
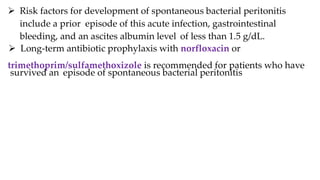
This document summarizes complications that can arise from cirrhosis and portal hypertension. It discusses hepatorenal syndrome, where renal failure develops due to renal vasoconstriction from advanced cirrhosis. It also covers hepatic encephalopathy, where confusion and other neurological signs appear due to liver disease. Finally, it examines portal hypertension complications like variceal bleeding, ascites, and hepatopulmonary syndrome where blood vessels in the lungs become enlarged due to high portal pressure.