This document provides an overview of the history and core principles of family medicine. It discusses:
- The development of family medicine as a specialty in the US and Nigeria in response to the decline of general practice.
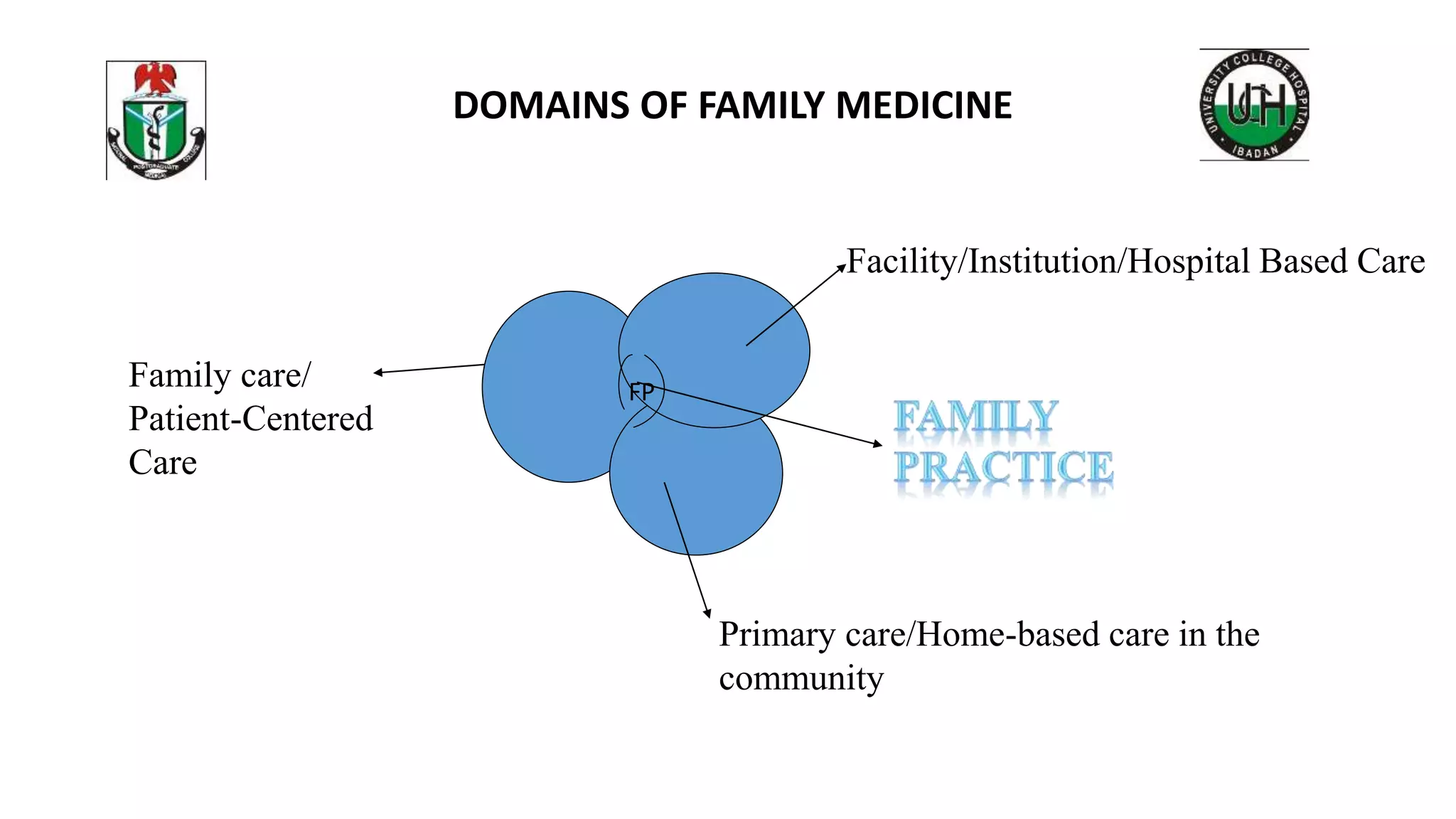
- The core domains of family medicine including family care, primary care, hospital/facility-based care.
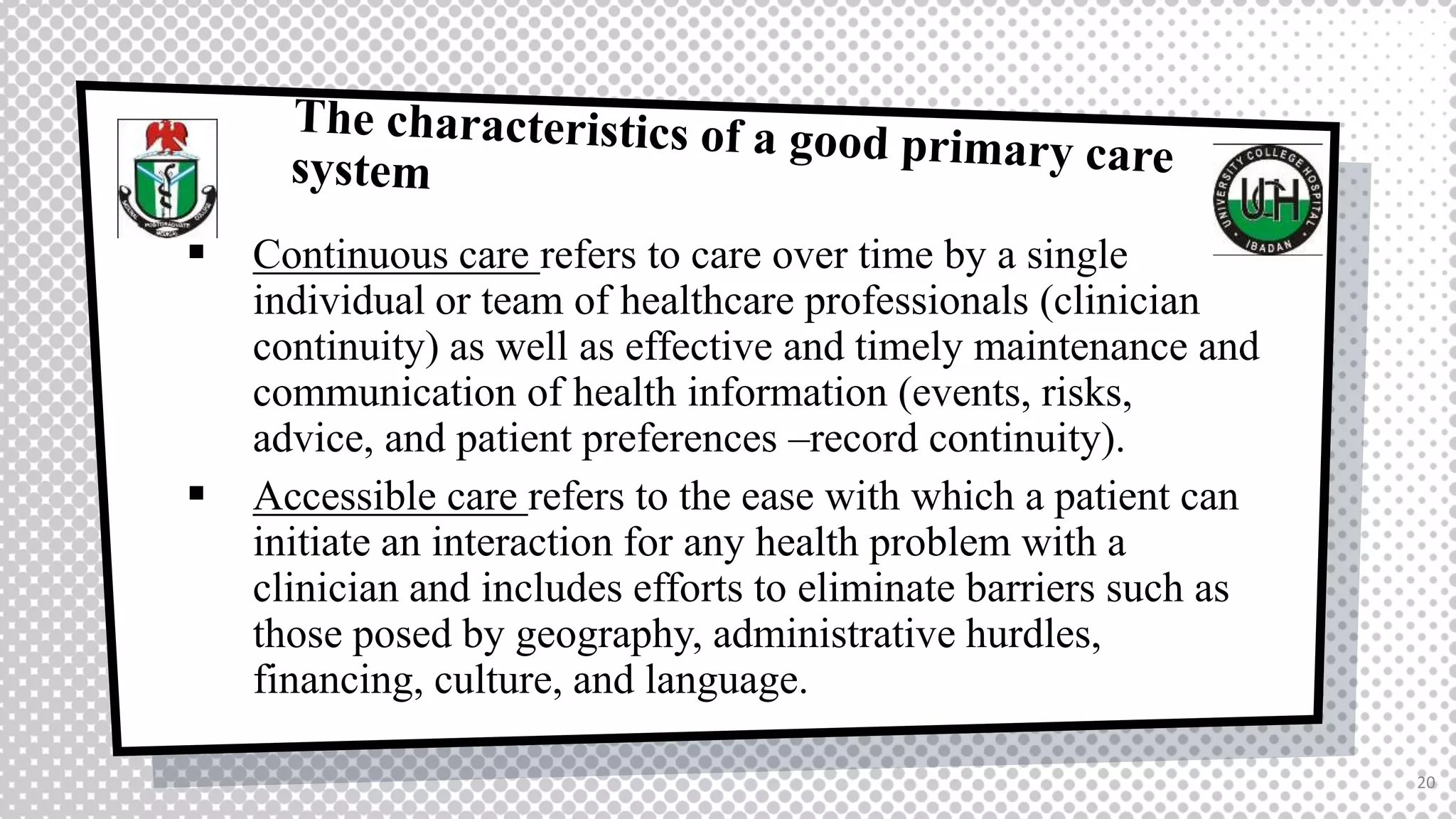
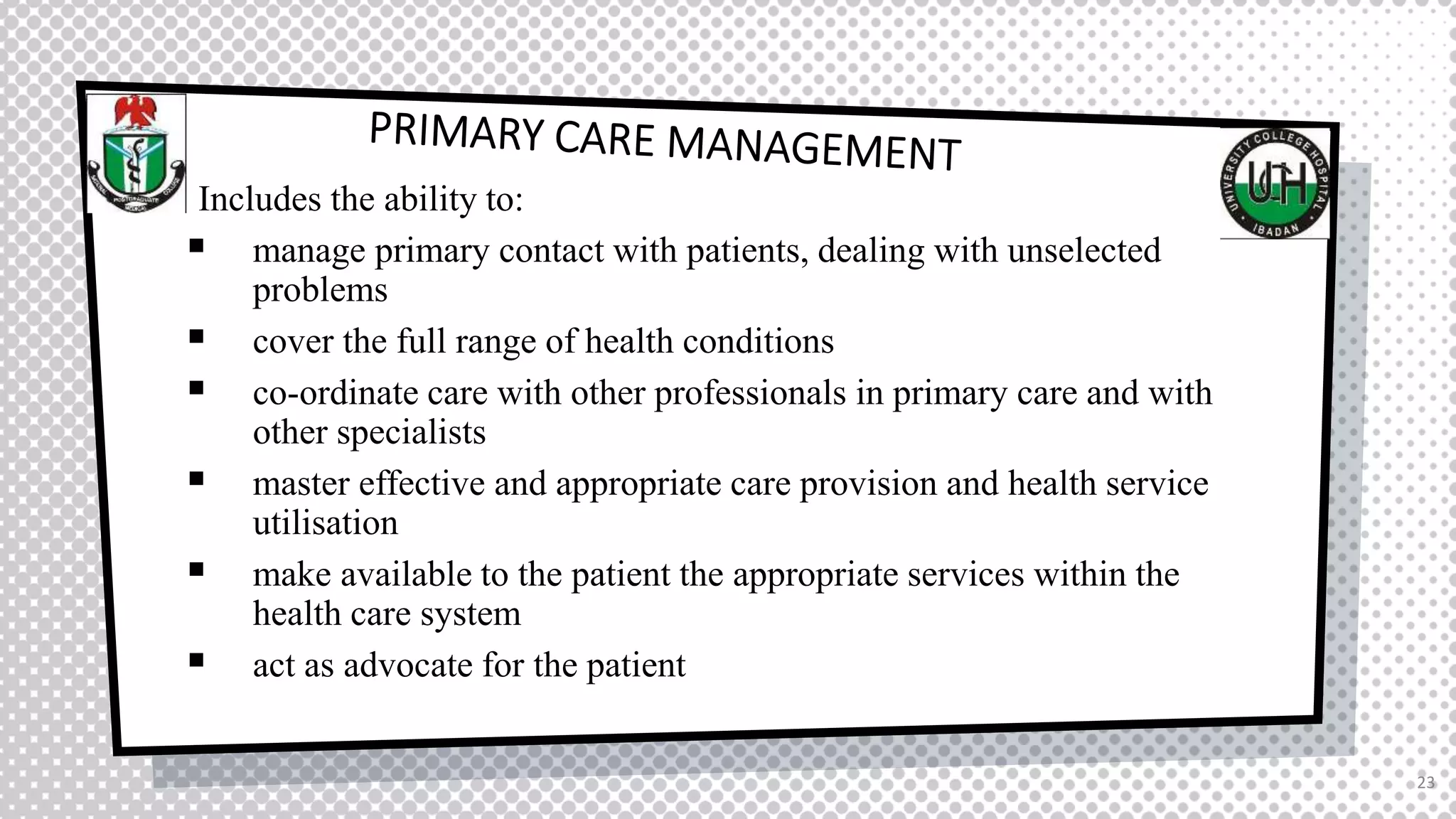
- The core competencies of family medicine according to the Wonca tree model including primary care management, person-centered care, problem-solving skills, community orientation, and a holistic approach.
- The definition of a family physician as a specialist trained to provide comprehensive care for individuals and families regardless of health issues.



































![REFERENCES
The European Definition of General Practice / Family Medicine Wonca Europe 2011 Edition
WHO, Family Medicine Report of a Regional Scientific Working Group Meeting on Core
Curriculum Colombo, Sri Lanka, 9-13 July 2003. http://apps.searo.who.int/pds_docs/B3426.pdf
http://www.sofpon.org/role-family-medicine-family-physicians-nigerian-health-sector/
Canfield, P. R. (1976). Family medicine. Academic Medicine, 51(11), 904–
11. doi:10.1097/00001888-197611000-00003
Seiyefa Fun-Akpa Brisibe,19 Inaugural Lecture Family Medicine: The complexities of
differentiating undifferentiated diseases in a differentiated profession. 2016
AV Inem, OO Ayankogbe, M Obazee, MM Ladipo, NE Udonwa, Kofo Odusote. What Constitutes
The Domain of Family Medicine in West Africa. 2004
Older Adults’ Needs and Preferences for Open Space and Physical Activity In and Near Parks: A
Systematic Review - Scientific Figure on ResearchGate. Available from:
https://www.researchgate.net/figure/The-biopsychosocial-model-of-health-
Source_fig2_321893403 [accessed 1 Jan, 2020]
39](https://image.slidesharecdn.com/coreprinciplesoffamilymedicine-221004105232-b43edfcf/75/Core-Principles-of-Family-Medicine-pptx-39-2048.jpg)
