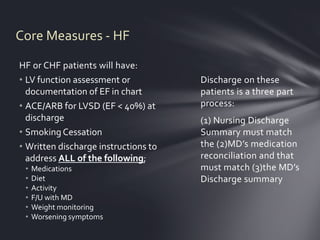
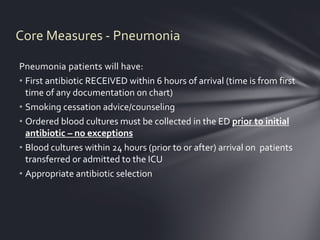
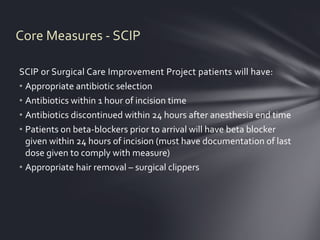
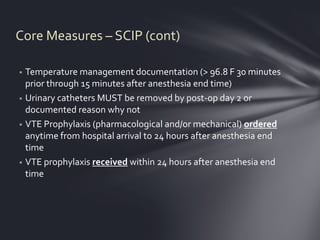
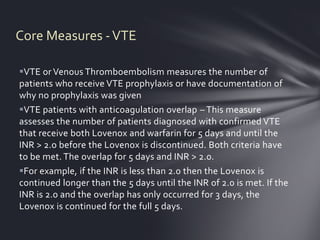
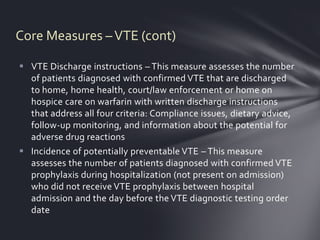
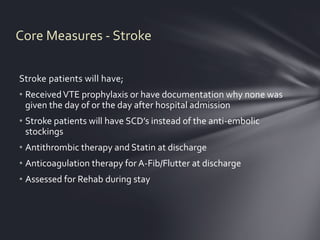
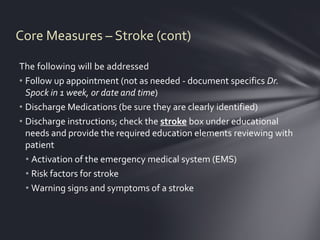
Core measures are evidence-based standards established by CMS to improve patient outcomes. Hospitals must report on core measures to receive reimbursement, and this data is publicly reported. At WCMC, teams monitor measures for conditions like AMI, HF, PN, surgery, VTE, and stroke. The red chart identifies patients for core measures, which staff must ensure are addressed according to guidelines. Measures include things like timely treatment, screening, counseling, and discharge instructions. Accurate documentation and coordination between staff is important for compliance.