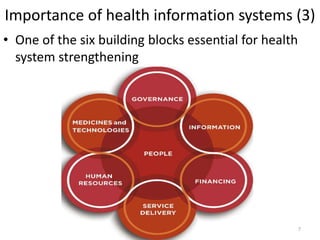
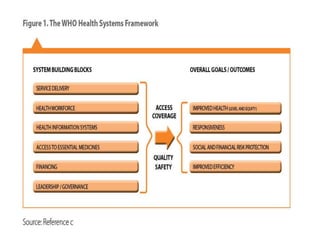
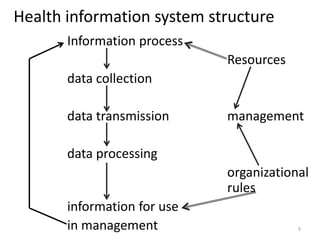
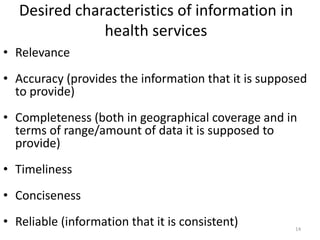
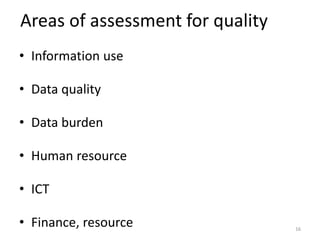
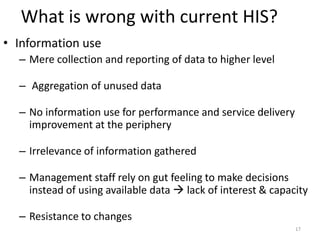
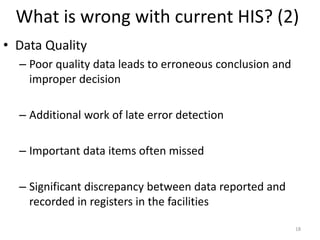
The document defines and discusses health information systems and their importance. It provides definitions of key terms like health information system, management information system, and health management information system. It outlines the importance of health information systems in supporting management functions, decision making, and health system strengthening. It describes the typical components and structure of health information systems, including data collection, management, and use. It also discusses issues that can undermine current health information systems and provides steps to develop and improve such systems.