Recommended
PDF
PPTX
PPTX
Conference ortho extณัฐดนัย
PPTX
Common respiratory problems
PPTX
PPTX
Avascular necrosis ug class
PPTX
Osteonecrosis of the femoral head
PPTX
PPTX
PPTX
PPTX
ortho conference 3 nov 2017
PPTX
Orthopedic conference Ext.จารุภา มงคลโชติการ 15 พ.ย.60
PDF
PPTX
PDF
Case conference orthopedic
PDF
PPTX
Case conference-by-extern-arichaya
PPTX
Orthopedic extern conference Ext.นรวิชญ์ 16 ก.พ.61
PPTX
PPTX
Case teleconference 30 พย.60
PPTX
PPTX
Orthopaedic teleconference
PDF
Non-infectious orthopedic problem for nursing students 2560
PDF
Intertrochanteric fracture (2)
PDF
Extern conference ปิติพงษ์ แสงสำฤทธิ์
PPTX
Externs conference Ext อิสสรีย์ พฤกษวิวัฒน์ รามา
PPTX
Extern conference.romthira
PPTX
More Related Content
PDF
PPTX
PPTX
Conference ortho extณัฐดนัย
PPTX
Common respiratory problems
PPTX
PPTX
Avascular necrosis ug class
PPTX
Osteonecrosis of the femoral head
PPTX
Similar to Conference เวชพิสิทธิ์
PPTX
PPTX
PPTX
ortho conference 3 nov 2017
PPTX
Orthopedic conference Ext.จารุภา มงคลโชติการ 15 พ.ย.60
PDF
PPTX
PDF
Case conference orthopedic
PDF
PPTX
Case conference-by-extern-arichaya
PPTX
Orthopedic extern conference Ext.นรวิชญ์ 16 ก.พ.61
PPTX
PPTX
Case teleconference 30 พย.60
PPTX
PPTX
Orthopaedic teleconference
PDF
Non-infectious orthopedic problem for nursing students 2560
PDF
Intertrochanteric fracture (2)
PDF
Extern conference ปิติพงษ์ แสงสำฤทธิ์
PPTX
Externs conference Ext อิสสรีย์ พฤกษวิวัฒน์ รามา
PPTX
Extern conference.romthira
PPTX
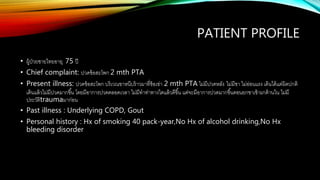
Conference เวชพิสิทธิ์ 1. 2. PATIENT PROFILE
• ผู้ป่วยชายไทยอายุ 75 ปี
• Chief complaint: ปวดข้อสะโพก 2 mth PTA
• Present illness: ปวดข้อสะโพก บริเวณขาหนีบร้าวมาที่ข้อเข่า 2 mth PTA ไม่มีปวดหลัง ไม่มีชา ไม่อ่อนแรง เดินได้แต่ผิดปกติ
เดินแล้วไม่มีปวดมากขึ้น โดยมีอาการปวดตลอดเวลา ไม่มีทาท่าทางใดแล้วดีขึ้น แต่จะมีอาการปวดมากขึ้นตอนยกขาเข้ามาด้านใน ไม่มี
ประวัติtraumaมาก่อน
• Past illness : Underlying COPD, Gout
• Personal history : Hx of smoking 40 pack-year,No Hx of alcohol drinking,No Hx
bleeding disorder
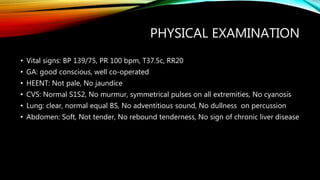
3. PHYSICAL EXAMINATION
• Vital signs: BP 139/75, PR 100 bpm, T37.5c, RR20
• GA: good conscious, well co-operated
• HEENT: Not pale, No jaundice
• CVS: Normal S1S2, No murmur, symmetrical pulses on all extremities, No cyanosis
• Lung: clear, normal equal BS, No adventitious sound, No dullness on percussion
• Abdomen: Soft, Not tender, No rebound tenderness, No sign of chronic liver disease
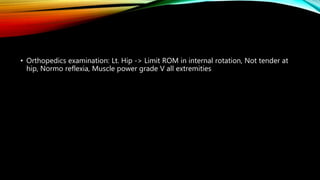
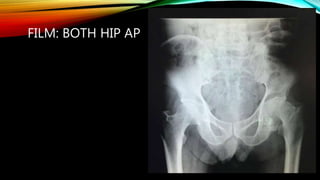
4. • Orthopedics examination: Lt. Hip -> Limit ROM in internal rotation, Not tender at
hip, Normo reflexia, Muscle power grade V all extremities
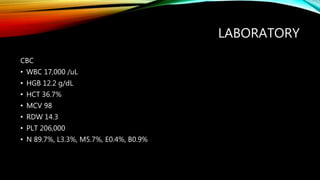
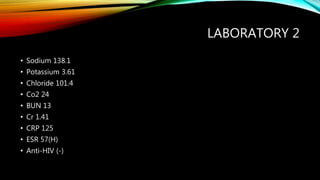
5. 6. LABORATORY 2
• Sodium 138.1
• Potassium 3.61
• Chloride 101.4
• Co2 24
• BUN 13
• Cr 1.41
• CRP 125
• ESR 57(H)
• Anti-HIV (-)
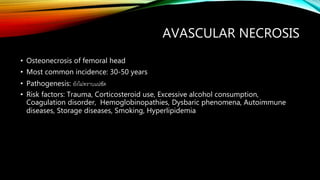
7. 8. 9. AVASCULAR NECROSIS
• Osteonecrosis of femoral head
• Most common incidence: 30-50 years
• Pathogenesis: ยังไม่ทราบแน่ชัด
• Risk factors: Trauma, Corticosteroid use, Excessive alcohol consumption,
Coagulation disorder, Hemoglobinopathies, Dysbaric phenomena, Autoimmune
diseases, Storage diseases, Smoking, Hyperlipidemia
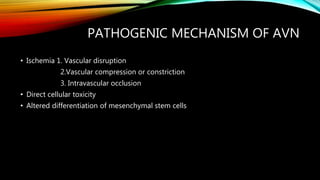
10. PATHOGENIC MECHANISM OF AVN
• Ischemia 1. Vascular disruption
2.Vascular compression or constriction
3. Intravascular occlusion
• Direct cellular toxicity
• Altered differentiation of mesenchymal stem cells
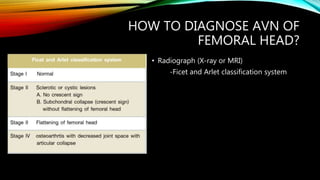
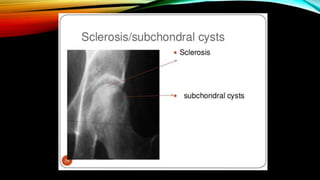
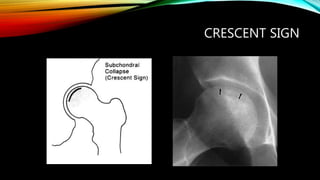
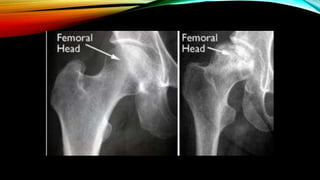
11. 12. HOW TO DIAGNOSE AVN OF
FEMORAL HEAD?
• Radiograph (X-ray or MRI)
-Ficet and Arlet classification system
15. 18. TREATMENT
• Non surgical treatment
1.Non-weight bearing therapy : For small and asymptomatic lesion
2.Biophysical modalities: ESWT(Extracorporeal shock waves therapy)
HBO(Hyperbaric )
3.Pharmacotherapy : Enoxaparin, Bisphosphonates
19. SURGICAL TREATMENT
• Femoral head-preserving procedure
1.Core decompression
2.Core decompression with nonvascularized bone grafting
3.Vascularized bone grafting
4.Concentrated stem cell
5.Biologic adjuncts
6.Tantalum rods
7.Rotational osteotomy
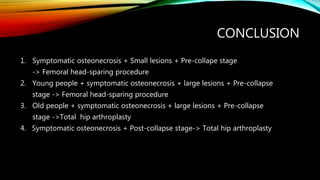
20. 21. CONCLUSION
1. Symptomatic osteonecrosis + Small lesions + Pre-collape stage
-> Femoral head-sparing procedure
2. Young people + symptomatic osteonecrosis + large lesions + Pre-collapse
stage -> Femoral head-sparing procedure
3. Old people + symptomatic osteonecrosis + large lesions + Pre-collapse
stage ->Total hip arthroplasty
4. Symptomatic osteonecrosis + Post-collapse stage-> Total hip arthroplasty