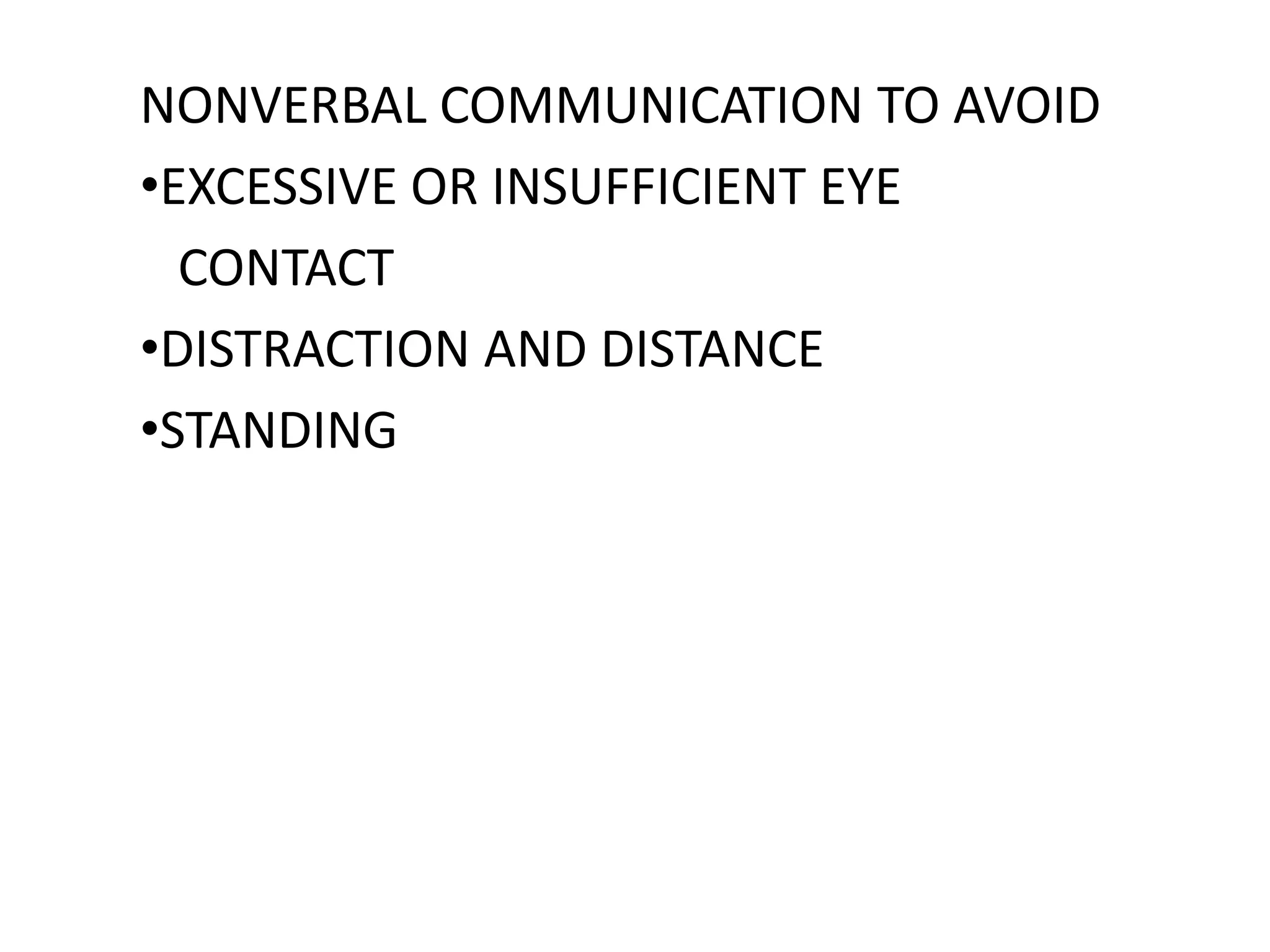
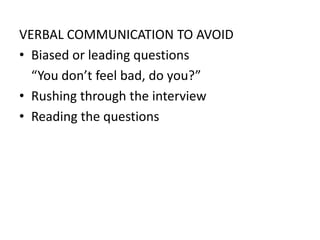
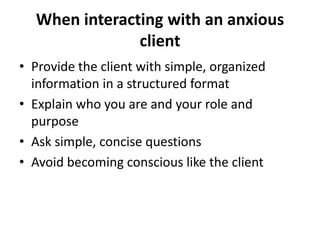
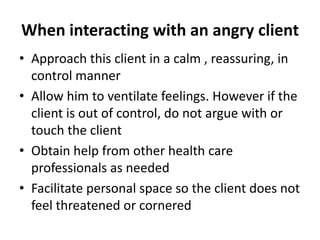
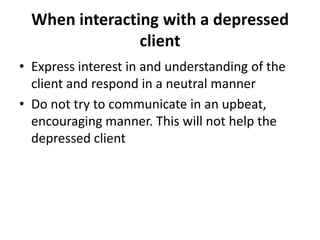
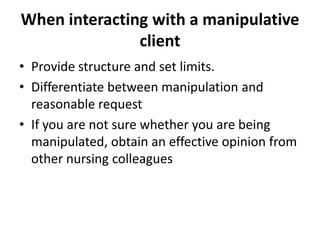
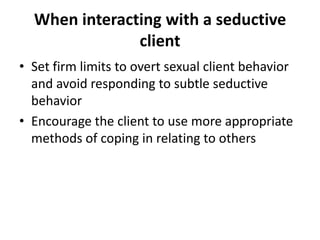
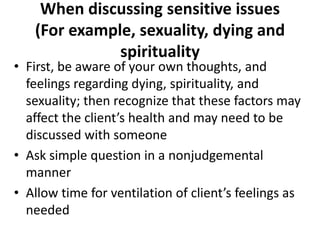
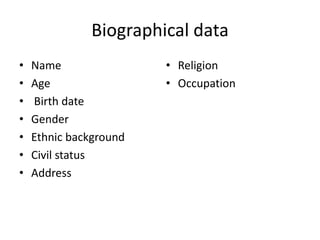
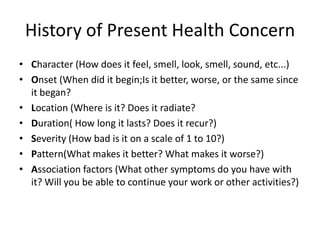
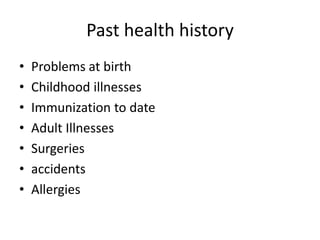
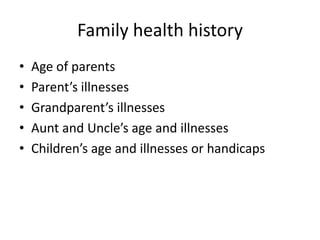
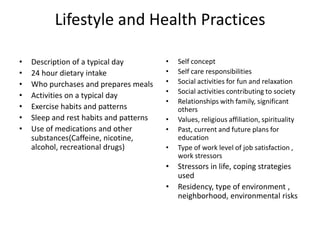
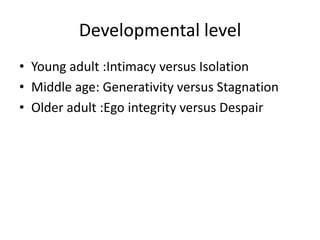
The document provides guidance on effective communication strategies when interacting with clients in different emotional states such as anxiety, anger, depression, manipulation, seduction, and discussing sensitive issues. It outlines best practices for nonverbal and verbal communication, asking questions, addressing client feelings, setting limits, and obtaining help from colleagues as needed for each client type. Guidelines are also given for collecting relevant biographical, health history, lifestyle, and developmental information from clients.